Navigating Panic Disorder: Understanding, Coping and Supporting
Navigating Panic Disorder: Understanding, Coping and Supporting

We regularly encounter stressful and challenging situations that can heighten our anxiety or fear. But sometimes, an experience can be particularly overwhelming, and our bodies react instinctively with a physical and emotional intensity that kickstarts our fight-or-flight response. Because of intrusive thoughts, it’s suddenly hard to breathe; we feel our heart racing or that we’re having chest pains and start sweating. Detached from our surroundings, while consumed by racing thoughts and a sense of impending doom, we feel like we’ve lost control. Panic attacks are highly distressing and disruptive.
When panic attacks begin to occur repeatedly, however, the person experiencing them might start to be consumed with worry about the potential and unpredictable nature of future episodes, so much so that the fear of that possibility begins to affect their behaviour and lifestyle significantly. This is known as panic disorder. In these situations, where a pattern of recurring panic attacks develops, it is essential to seek professional help.
In this article, we’ll look at the concept of a panic attack versus panic disorder. Not everyone who experiences a panic attack will have panic disorder, but those with panic disorder will often experience repeated panic attacks. Panic attacks can occur with any anxiety disorder as well as other mental disorders (e.g., PTSD, substance use disorders, depressive disorders) and some medical conditions (e.g., cardiac, gastrointestinal, respiratory, vestibular). We’ll explore the relationship with agoraphobia, discuss some treatment options and coping strategies that can help support someone with greater empathy and understanding. From there, we’ll also address how veterans can be at increased risk of developing panic disorder and share resources that are essential to creating a supportive environment and helping to destigmatize mental health concerns.
What is panic disorder?
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), panic disorder can be diagnosed when someone frequently experiences recurring and unexpected panic attacks and is persistently worried about having more panic attacks or changes their behaviour in maladaptive ways because of the panic attacks (e.g., avoidance of exercise or of unfamiliar locations). (1) Panic disorder is not the same as an anxiety or a panic attack, though both can be elements of this type of mental health condition.
| Anxiety | Panic Attack | Panic Disorder |
| Feeling uneasy | A sudden, intense surge of fear | Repeated, unexpected, and unpredictable panic attacks. |
| Constant worry about having future panic attacks can heighten anxiety. | ||
| Intense and overwhelming feeling of losing control.Persistent fear that something terrible will happen during a panic attack. | ||
| Example: You might feel anxious before taking a test or making an important decision. | Example: You might experience a panic attack if you are afraid of heights and go on a Ferris wheel. | Example: You might be experiencing panic disorder if, during a panic attack, you feel intense physical and emotional symptoms. Your pulse might start pounding so intensely that you begin to think you are having a heart attack. It could lead to waves of successive or simultaneous panic attacks where you start to feel short of breath and dizzy or begin to sweat and have abdominal pain. You may be unable to determine the cause of your panic attacks because no obvious danger could have triggered them. You will often start to worry about when the next attack will happen. There could be more today, this week, or this month. |
Panic disorder can make daily life challenging and can affect a person’s comfort with social interaction. They may prefer to stay within what they determine to be a safer environment where they are close to exits and have ways to escape a situation if a panic attack does happen. There may be a lot of pre-planning for outings, so they feel prepared by having medication or trusted friends and family members nearby. What someone with panic disorder is experiencing is real and should never be thought of as an overreaction.
It’s important to note that not everyone who has experienced anxiety or had a panic attack will go on to develop panic disorder. It’s estimated that:
-
- While up to 1/3 of Canadian adults may have a panic attack, about 4% of them will experience panic disorder in their lifetime (2)
-
-
- Up to 11% of people in the US experience a panic attack (3)
-
-
- Approximately 2-3% of them have panic disorder (4)
-
-
- Onset often occurs in the late teens and early twenties (5)
-
-
- It often affects women more than men (6)
Signs and Symptoms
Panic attacks can vary in their abrupt peak of intense fear or intense discomfort and peak in intensity within a few minutes. (7) People can experience physical symptoms like:
-
- Racing heart
- Shortness of breath
- Trembling
- Chest pain
- Dizziness
- Sweating
-
Emotionally, someone may feel intense fear, impending doom or like they have lost control. It’s important to note that for the person going through a panic attack, their perception of time can be distorted, making the experience feel much longer.
With panic disorder, frequency, intensity, and duration help determine different degrees and classifications of symptoms: (8)
| Type 1 | Type 2 | Type 3 | Type 4 |
| A single panic attack. | Frequent panic attacks (without depression). | Regular and recurring attacks with the gradual development of additional symptoms such as anticipatory anxiety, general anxiety, or agoraphobia. | Recurring panic attacks with additional symptoms, including depression. |
The Relationship with Agoraphobia
Agoraphobia is intense anxiety because of thoughts about being in situations or places where it can be difficult to leave or get help. The spaces are usually either open “such as parking lots, marketplaces, bridges) or enclosed, “such as tunnels, small rooms and elevators,” as well as “supermarkets, shopping malls and other crowded places,” including public transportation and unfamiliar environments. (9) People experiencing agoraphobia can feel trapped, helpless, or embarrassed as the worry that they may experience a panic attack overwhelms them. In some cases, someone experiencing panic disorder with agoraphobia “may not be able to leave the house.” (10) While symptoms of agoraphobia can exist without experiencing a panic attack, with panic disorder, there is no apparent reason for the agoraphobia to be present.
Veterans and Panic Disorder
Veterans can be at increased risk of developing panic disorder and substance use disorder due to the nature of their roles and exposure to combat, traumatic experiences and heightened general stress they experience during deployment. Programs like the Guardians Program, https://homewoodhealthcentre.com/treatment-programs/guardians-program/, at the Homewood Health Centre can offer specialized mental health support for veterans.
Treatment Options
There are a few treatment approaches that are effective to help with panic disorder. Working with a doctor is the best place to start, as they can help you understand what might work well and consider combinations that could provide relief more rapidly.
| Psychotherapy | Medication | Complementary and Alternative Therapies |
| Cognitive-Behavioural Therapy (CBT)Helps identify symptoms and triggers, plus develop ways to cope and change behaviours. Exposure Therapy Helps address associations between fears and bad outcomes to help manage anxious feelings. | Depending on which medications your doctor might recommend, relief can happen within a few weeks. Some medicines may take longer to see improvements. Your doctor will discuss possible side effects and work to find a medication that works. | Art therapy Breath training Both types of treatment can be helpful. Because they help reduce stress, plus develop calm and healthy mindfulness and self-regulation techniques when you practice them. Sometimes, these methods are easier for people to use to help them complete any ‘homework’ from psychotherapy treatment. |
Coping Strategies
Meditation and lifestyle choices such as prioritizing better sleep, regular exercise, a balanced diet and limiting alcohol intake, plus maintaining social connections, are always good ways to cope with life’s stressful situations. Some specific techniques can be helpful to try when experiencing anxiety or panic attacks:
- Breathing and relaxation techniques can help regulate the body’s stress response by introducing a rhythm that helps calm our automatic nervous system responses and reduce anxiety.
- The 555 breathing technique involves inhaling for a count of 5, holding the breath for a count of 5 and then exhaling for a count of 5.
- Box breathing is similar in that it involves inhaling for a specific count, holding the breath for the exact count, and exhaling for the same count. With box breathing, you add a counted pause before starting the cycle. Practitioners sometimes suggest envisioning a box shape to complete the technique.
- Mindfulness practices that help focus on sensory awareness and offer grounding can also help during a panic attack and promote overall well-being. These exercises can help shift attention away from anxious thoughts.
- The 333 sensory awareness technique involves identifying and acknowledging three things you can see, three things you can hear, and three things you can touch in your immediate surroundings.
- The 54321 technique is similar but includes even more sensory awareness. You focus on naming five things you can see, four things you can touch, three things you can hear, two things you can smell and one thing you can taste.
How to Support Someone During a Panic Attack
- Understand the nature of a panic attack and remember you are there to support someone experiencing one.
- Remain calm and provide reassurance, emphasizing that the panicked feelings will pass. Talk using short sentences.
- Encourage the person to use coping strategies that they may have learned in therapy or that you are aware of, like mindful breathing and grounding techniques. Even simply helping them count slowly aloud to ten can help slow their heart rate and make them more responsive.
-
-
-
Developing awareness and understanding of panic disorder is crucial to fostering compassion, being supportive and eliminating stigma around mental health. Knowing some signs and symptoms can help all of us create a better sense living in a supportive community.
References:
1. American Psychiatric Association. (2013). Anxiety disorders. Retrieved January 12, 2024 from Diagnostic and statistical manual of mental disorders (5th ed.).
2. Canadian Mental Health Association – British Columbia Division (n.d.). Panic Disorder. CMHC BC. Retrieved January 1, 2024 from https://bc.cmha.ca/documents/panic-disorder-2/
3. Cleveland Clinic (medically reviewed) (2023 Feb 12). Panic Attacks & Panic Disorder. Cleveland Clinic. Retrieved January 1, 2024 from https://my.clevelandclinic.org/health/diseases/445…
4. Ibid.
5. Burke D., and Collins D. (medically reviewed) (2022 Feb 23). A guide to Panic Attacks and Panic Disorder. healthline. Retrieved January 1, 2024 from https://www.healthline.com/health/panic-disorder
6. Ibid.
7. American Psychiatric Association. (2013). Anxiety disorders. Retrieved January 12, 2024 from Diagnostic and statistical manual of mental disorders (5th ed.).
8. Takeuchi, T. et al. (2022 March). Four clinical types of panic disorders – Abstract. National Library of Medicine. Retrieved January 1, 2024 from https://pubmed.ncbi.nlm.nih.gov/1635333/#:~:text=T…
9. Antony, M. Ph.D. (2002). Panic Disorder and Agoraphobia. St. Joseph’s Healthcare Hamilton. Retrieved January 1, 2024 from https://www.stjoes.ca/health-services/mental-healt…
10. Ibid.
Good Food, Good Mood: The Link Between Nutrition and Mental Health
Good Food, Good Mood: The Link Between Nutrition and Mental Health

Our brains are hungry. In fact, brain cells are by far the hungriest cells in our bodies. They make up only 2% of our body weight, but use about 20% of the food energy we take in. And that energy goes toward our mental health as much as our physical health.
Many of us have experienced the close link between nutrition and mental health when we get “hangry,” that hunger-fueled mix of anger and irritability that consumes us when we skip a meal or forget to pack a snack.
But that’s just the tip of the iceberg. In fact, nutrition has a crucial role to play in protecting and improving our mental health, or even helping us manage a mental illness such as depression, anxiety, or trauma.
For the past five years, Marianne Bloudoff, BSc, a registered dietitian, has made nutrition and mental health the focus of her work at Homewood Ravensview, a private mental health and addiction treatment centre on Vancouver Island, British Columbia.
“A well-nourished brain is more focused, better able to handle stressors, and ensures a more stable mood,” Bloudoff explained. “You need those building blocks to create a foundation for the recovery journey.”
In this article, she explains the link between nutrition and mental health, and shares some of her tips for using nutrition to support better mental health.
From good food to good mood
Food components help the body create neurotransmitters, such as dopamine and serotonin (the so-called “happy hormones”), which alleviate anxiety and depression and boost mental health.
These neurotransmitters are sensitive to food intake, so changes in our eating patterns can have effects on behavior, sleep, and energy levels. The way we eat can also improve the effectiveness of medications, including antidepressants.
The food we eat can also help our mental health by ensuring that we build a healthy microbiome. This is what we call the 100 trillion bacteria—some helpful, some harmful—that can be found in the gut. When we eat probiotics and fermented foods that contain healthy bacteria (yogurt and kimchi are two examples), we can create a healthier, more resilient microbiome. This, in turn, creates a healthy feedback loop between our bodies and minds. Good food produces a good mood, and that in turn reduces the stress that can disrupt our digestive processes and prevent our gut from absorbing and metabolizing nutrients. As an interesting example of this phenomenon, Bloudoff pointed out that 26% of people with anxiety disorders have a digestive condition called irritable bowel syndrome (IBS).
Simplifying good nutrition for mental health
Mental health can complicate nutrition. When people are depressed, they may not have an appetite or the energy to source and prepare healthy foods. ADHD can make it difficult to plan, shop for, or prepare meals. Substance abuse can add another layer of difficulty to the issue.
But that doesn’t mean good nutrition has to be complicated. In fact, Bloudoff tries to make it as simple as possible for her patients to eat nutritious diets by making sure her recommendations take into account their unique needs and lifestyle.
“Every patient is different, so it’s about finding what works for the person,” she explained. “What is their reality? What kind of food can they afford? What do they have access to? What’s culturally appropriate for them? What do they like? Are they feeding just themselves or a whole family? Do they have allergies? What do they know how to prepare? One person might live in a big city close to a supermarket. Another might live in a rural area where they fish or hunt.”
By taking into account the individual’s broader context, including their background, geography, culture, family status, strengths and capabilities, community support, and more, she can ensure the foods she recommends to her patients will be easier and more intuitive for them to source, prepare, and enjoy.
Eat these key nutrients for brain health
While there’s no universal diet for good mental health, there are specific nutrients that everyone needs to ensure they consume in order to lay the groundwork for a healthier body and mind.
Omega-3 fats
Omega-3 fats can be found in oily fish, such as salmon and sardines, and plant sources such as walnuts, flax seeds, and chia seeds. Omega-3 fats build brain cell membranes, reduce inflammation, and promote new brain cell formation, which can improve mood and memory, and reduce the occurrence of brain disorders.
Complex carbohydrates
These can be found in whole grains, legumes, fruits, and vegetables, and our bodies break them down slowly so they deliver energy consistently over a longer period of time. Eating meals or snacks that include complex carbs every three to five hours can contribute to a more stable, happy mood.
Vitamins
You’ll find B vitamins in meat, dairy, eggs, whole grains, beans, nuts, seeds, and leafy green vegetables, while vitamin D can be found in eggs, meat, and oily fish. Deficiencies in vitamin B12 can cause depression, irritability, agitation, psychosis, and decrease antidepressant response, while deficiencies in vitamin D have been found in people with depression, seasonal affective disorder, and schizophrenia.
Minerals
Iron, magnesium, and zinc are all minerals associated with brain health. Iron stimulates brain development and protects against dementia, while magnesium is associated with improved sleep, and both magnesium and zinc help to protect against depression. Meat, fish, beans, nuts, seeds, and leafy greens are good sources of iron, while pumpkin and flax seeds, almonds, cashews, avocado, tofu, spinach, swiss chard, and black beans all contain magnesium. Zinc can be found in oysters, crab, beef, pork, chicken, and beans.
Antioxidants
Antioxidants include vitamin C, vitamin E, carotenoids, and flavonoids, which can be found in all fruits and vegetables. These nutrients help the brain fight oxidative damage and neural inflammation by preventing harmful free radicals from forming. This helps to protect the brain against neurodegenerative disorders, anxiety, and depression.
Amino acids
Tryptophan is an amino acid needed to produce serotonin, a neurotransmitter that promotes sleep, calmness, and relaxation. Another amino acid, tyrosine, is needed to create the neurotransmitters dopamine and norepinephrine, which create feelings of pleasure and improve motivation, alertness, and focus. Tryptophan and tyrosine can both be found in protein-rich foods including nuts, seeds, tofu, cheese, yogurt, meat, fish, beans, lentils, and eggs.
Water
You may not think of it as a nutrient, but water is essential to healthy brain function. In fact, a mere 1% drop in hydration is associated with a 5% drop in cognitive function, while a 2% drop can cause short-term memory impairment and difficulty focusing. Drinking enough water and getting hydration from other food and beverage sources helps us stay alert.
Being nourished as well as fed
The connection between nutrition and mental health goes beyond getting enough of the right nutrients. It has emotional, social, and cultural dimensions that can nourish us in deep and meaningful ways, and Bloudoff said these aspects are just as important to our mental health. That’s why she stresses the importance of eating for enjoyment, meaning, and connection.
“The foods we choose and our eating experiences also impact our emotional health,” Bloudoff explained. “We have emotional and cultural connections to food, and we connect with others over food.”
Eat together
Eating with others has many benefits, including building social connections with family, friends, coworkers and exploring new foods you might not normally try.
“Whether it’s the classic, nuclear-family meals on Sunday night or meeting up with friends for coffee and a snack, these are ways to foster emotional and mental health.”
Eat for pleasure
Including foods we enjoy in our diets can promote positive emotions, and it also motivates us to seek food out regularly enough that we stay nourished and energetic. Cultural or traditional foods, especially, can help us strengthen personal and cultural connections as well as delivering important sources of key nutrients.
“Food is more than just fuel. When it’s pleasurable, culturally appropriate, and meaningful, it’s going to make you feel good on more levels than just the physical.”
A vital piece of the puzzle
Recovery is a complex and multifaceted process, and nutrition is one of many aspects that impact mental wellness. At Homewood Ravensview, Bloudoff works alongside physicians, nurses, psychiatrists, therapists, addictions counsellors, occupational therapists, and recreation, horticulture, music, and art therapists. But good nutrition can set the stage for success across the wellness journey.
“Nutrition doesn’t replace therapy or medications, but they all work together holistically,” she explained. ” Medications don’t work properly if you don’t have adequate nutrition. Therapy may not be as effective if you’re not feeding your brain so you can give it your focus and energy. Nutrition is one of those foundational pieces that help us do all the things that are important from a mental health perspective.”
Interconnections Between Stress, Diabetes, Nutrition, and Mental Health
Interconnections Between Stress, Diabetes, Nutrition, and Mental Health

Most people know that stress is something to reduce or avoid, but it may be surprising to learn how much it can affect our overall health and well-being. It’s especially true for people who are living with metabolic diseases like diabetes.
Stress significantly affects our body’s ability to stabilize blood sugar levels and reach a manageable state. What’s perhaps more problematic is that it’s thought that close to 40% of those with diabetes are unaware they have it. (1) When imbalanced and uncontrolled, diabetes can lead to various complications, including cardiovascular disease (stroke and heart disease), kidney problems and nerve damage.
This article will look at the interplay and relationships between stress, nutrition, diabetes, and mental health. With a better understanding of how everything is connected, we can explore some early warning signs that could make you want to determine your diabetic status. From there, we can share some tips to help you think about how stress might affect how your body processes glucose and determine how to reduce stress overall for better health.
How does stress affect blood sugar levels?
When stressed, cortisol and adrenaline are released into our bodies, prompting our pancreas to release stored glucose into our bloodstream. It’s a natural response: these hormones raise blood sugar to react to a fight-or-flight situation. This happens in a fraction of a second and starts a complex sequence of events. (2)
When our bodies perceive a threat, this instinctive reaction gives us the quick energy we might need to survive it. At the same time, we need to be able to lower blood sugar levels when we aren’t under threat to ensure that all our cells have the necessary energy to function correctly. Insulin is the chemical signal responsible for regulating glucose and determining how we store nutrients in our liver and muscles. It also plays a significant role in how our bodies hold fat molecules. Being in a state of chronic stress can lead our bodies to develop a state of chronic inflammation and is linked to a condition referred to as insulin resistance.
Chronic stress doesn’t allow for the natural conditions to have insulin work to clear away elevated levels of stress hormones within our bodies. Over time, cells become less responsive to insulin while it tries try to simply do its job as the natural chemical messenger it is. When that happens, our bodies pay less attention to those signals, and how we absorb and clear glucose in our bloodstream becomes impaired. Since insulin is such an essential energy regulator, improper functioning can affect our overall health in ways we don’t realize.
How is nutrition related?
Our bodies operate on a delicate balance of carbohydrates, proteins, and fats, where each nutrition element is critical to our overall well-being. When there are imbalances from having either too much or too little of these nutrients, it can impact our health because our body’s priority is to protect the brain. Nutrition is also linked to stress levels and blood sugar regulation. Sometimes, we may use emotional eating or binge eating as coping mechanisms to try and address high stress.
Discovering how much our gastrointestinal system plays a part in our emotional health can be surprising. Researchers have learned that “a big part of our emotions are probably influenced by the nerves in our gut.” (3) As part of the digestive process, the microorganisms that live in our gut produce neurotransmitters like serotonin. Serotonin is closely related to mood and emotional well-being. Imbalances can contribute to depression and anxiety, which can affect our overall emotional state. It gives some validity to our “gut feelings” because “95 percent of the body’s serotonin is found in the bowels,” so it makes sense for us to become more aware of our complex relationship with food. (4)
Some strategies could help develop greater awareness of the interconnectedness of food and how our bodies function under stress: (5)
1. Think about whether you have consciously or unconsciously established rules for when you can eat or what you can eat. If you recognize some, consider when these started and why.
2. Relearn your “natural hunger cues” to help you listen to what your body says about what it needs and when it’s full.
3. Slow down and savour your food choices by noticing the flavour, textures, and feelings you experience as you eat.
- Are you enjoying the food?
- Are you responding to a craving?
- Is eating solving the problem you may have started with?
- Is your hunger going away as you eat?
- Do you feel happy, guilty, or upset while eating?
When we recognize these thought patterns, we can understand how we behave around food and be more conscious that this act to nourish ourselves is only part of a series of processes activated in our bodies.
Symptoms of stress and diabetes
Since so many are living with undiagnosed diabetes and may be unaware of the relationship between the disease and chronic stress, we thought it might be helpful to share some signs to watch for. Please keep in mind that this information is never intended to replace a diagnosis or treatment plan recommended by a health care professional.
Here are some similarities and differences between Type 1 and Type 2 diabetes:
Note: We aren’t covering other related forms of diabetes such as gestational diabetes or pre-diabetes.
We often overlook or dismiss symptoms because our lives are hectic, so and stress is so prevalent. Here are some signs of stress and what we tend to attribute them to:
Consistent and comprehensive monitoring with your healthcare team helps you identify patterns and assess how stress affects you. With this information, you can make informed plans for addressing supportive changes.
Ways to reduce stress
Reducing stress is possible by using simple but effective strategies. Embracing these adaptations to your lifestyle can make a significant difference in your long-term health and well-being.
1. Get up and move around every day.
Spend at least 150 minutes each week doing activities that increase your heart rate and get your muscles moving. You don’t have to run or do things that cause extreme exertion, and you don’t have to do marathon sessions. Tasks around the house get you moving, too. Even ten minutes of walking helps. Movement has the added advantage of improving mental health too. Before long, you may notice that your body craves it!
2. Consume a wide variety of nutritious foods that provide your body with the vitamins and minerals that chronic stress can deplete.
Getting these through food sources rather than supplementation is always preferred. You should consult a doctor or pharmacist before taking supplements to try and counteract the effects of stress or prevent diseases. Doing so could inadvertently cause more internal stress and inflammation in your body that you are unaware of and create circumstances where your body may become more vulnerable to other diseases.
3. Reduce and redirect the time spent using social media in favour of connecting with other people.
You’ll be able to practice the art of friendship, learn from other people’s perspectives, and discover what it’s like to be an active part of a community. You could participate in shared activities, interests, or experiences.
4. Explore the mechanism of your breath.
It’s easy to start by first discovering how many times you breathe in one minute and then seeing if you can reduce that by breathing fuller, deeper, and with more awareness. How do you feel when you slow your breathing down? You might prefer to use guided meditations to help your breathing and visualize what calmness is for you.
5. Seek professional help and leverage counselling to address the root causes of chronic stress you may be experiencing.
Learning about yourself and your reactions can make you better informed and anticipate and plan a better response when you encounter a stressful situation.
Discovering more about how stress and blood sugar are interconnected is a way to manage and promote good health practices and gain knowledge to live a better life.
References:
1. PAHO (Pan American Health Organization, a branch of the WHO – World Health Organization). (2022 November 11). The number of people with diabetes in the Americas has more than tripled in three decades, PAHO report says. PAHO. Retrieved December 1, 2023 from https://www.paho.org/en/news/11-11-2022-number-peo…
2. ]Cleveland Clinic (2021 December 10 – last medical review). Cortisol. Cleveland Clinic Articles. Retrieved December 1, 2023 from https://my.clevelandclinic.org/health/articles/221…
3. Mayar, E. (as cited by Hadhazy, A.) (2010 February 12). Think Twice: How the Gut’s “Second Brain” Influences Mood and Well-Being. Scientific American. Retrieved December 1, 2023 from https://www.scientificamerican.com/article/gut-sec…
4. Ibid.
5. Davidson, K. MScFN, RD, CPT (medically reviewed by Seitz, A. MS, RD.). (2020 December 3). How Can I Improve My Relationship with Food? Healthline – NUTRITION. Retrieved December 1, 2023 from https://www.healthline.com/nutrition/fixing-a-bad-…
The Psychology of Debt
The Psychology of Debt

Debt can have a significant effect on our mental well-being. When the constant pressure of financial obligations and the anxiety of meeting payments looms over our heads, it can have an impact on our stress level, sleep and mood. It’s a burden that can even affect our self-esteem, making us feel insecure, inadequate, and helpless.
Our mental, physical, and financial health are connected, and we need to recognize how financial worries weigh on us so we can seek support to alleviate the stress and improve our mental health.
In this article, we’ll examine how debt affects us emotionally, influencing how we behave and how it makes us feel about ourselves. We’ll also connect the dots to what the strain of debt does to us physically. Once we have a better understanding of how it’s all connected, we can explore practical options and strategies that can be helpful to work on reducing and eliminating debt. It’s not a situation anyone intentionally ends up in, and it can be frightening. Taking small steps forward can help us feel a sense of direction again, regain control, and reduce stress to find a better balance between our health and wealth.
When it comes to finances, does everyone start from the same place?
Unfortunately, there is no equal ground when it comes to financial matters because disparities between resources, opportunities, and education all factor significantly into our individual experiences. It is an important reality to recognize as we consider the relationship between debt and mental health.
Contrasts and inequality around the economic circumstances we are born into create complexities that undeniably affect people’s well-being. Just think about the significant differences in housing, our environments, who we interact and form relationships with, and how we develop and identify ourselves. There needs to be more self-awareness regarding individuals’ advantages, benefits, or access to opportunities.
The interconnectedness of all kinds of social determinants, such as the affordability and availability of food and the reliability of transportation, affects someone’s ability to access essential services. People with economic privilege have higher levels of education and can typically make healthier lifestyle choices, in addition to having improved access to high-quality healthcare.
How does financial worry, particularly related to managing debt, affect mental health?
Feeling economically stable and secure can be a marker of financial success and is crucial to maintaining a positive and balanced view of life. For many people, trying to improve their earning potential starts as they enter adulthood, where education and skill development are often the priority, while at the same time, they are trying to manage living expenses. Despite knowing that budgeting and saving are habits to master in this phase of life and can certainly be helpful to set the stage for an easier time financially, they can be challenging to put into practice. Many psychological influences often need to be factored into the equation rather than simply focusing purely on “income and expenses.” (1)
Even though we might not have stable income and expenses, there are times when we focus on “wants” or things we aspire to. We convince ourselves that we’re depriving ourselves of experiences or the lifestyles we “deserve.” It’s at that moment that impulsive spending can happen. We start to spend because we feel bored or stressed, even though we don’t really have the financial means. And while those purchases might temporarily relieve those feelings, they set a course that contributes to long-term financial strain and unmanageable debt loads.
Over time, debt can make us feel overwhelmed and create intense pressures that affect our mental health and start to show up as:
-
- Anxiety
- Stress
- Frustration
- Depression
Our relationships can also take a toll, creating increased family tension and straining friendships. It affects how we communicate and our emotional well-being. We might feel embarrassed or full of shame for getting into the circumstances, which can lead to low self-esteem and a general feeling of helplessness.
Prolonged financial strain can even affect our physical health as our body responds to chronic stress. We can experience sleep problems, headaches, and digestive issues. Mentally, we may have reduced concentration and impaired decision-making abilities. It may seem easier for some to cope by avoiding what’s happening altogether, ignoring bills, and discussing money or financial responsibilities.
What kinds of drivers can influence our financial behaviours?
A complex combination of internal and external factors can influence how we handle financial decisions and manage money. Attitudes towards risk, biases we have, and financial literacy all come into play.
Economic conditions
The economy is shaped by inflation and interest rates, employment levels, and government policies that evolve and change over time. They are also largely out of our control. With periods of economic uncertainty, we tend to pay more attention to finances, prioritize essential expenses and savings over spending, and put off major purchases to be more budget-conscious and cautious about taking on additional debt.
It can be tough for many people who are watching their spending. Basic housing, food, transportation, and education costs are at all-time highs. For many, wages are stretched to their limits. Consumer Affairs researched costs between generational groups and found many alarming realities through their comparisons: (2)
-
- Those in Gen Z (born between 1996 and 2012) and millennials (born between 1981 and 1995) “are paying nearly 100% more for their homes than baby boomers [born between 1946 and 1964] did when they were in their twenties.”
- Gen Z dollars have “86% less purchasing power” than when baby boomers were in their twenties.
- Gen Z and millennials pay “nearly 60% more” than baby boomers in their twenties for gasoline.
- Many younger adults are priced out of the market because housing costs (when adjusted for inflation) are “nearly double” compared to when baby boomers were the same age.
- Today, rents are 150% more than in 1970, making saving difficult. Some rentals are “just as costly, if not costlier, than a mortgage.”
Job loss
Job loss can introduce heightened financial insecurity and stress due to fear and uncertainty. The loss of income may lead to a reassessment of priorities during unemployment. It can also increase anxiety.
Medical emergencies or illnesses
Unexpected healthcare expenses can accumulate quickly and profoundly impact financial well-being. Without adequate insurance coverage, people can face substantial medical bills, leading to increased debt, more financial strain, and potentially long-term consequences for overall financial stability. People may need to take a Leave of Absence (LOA) to care for a loved one or themselves and in turn can be impacted. It can be frightening, disheartening, and exhausting to worry about how to cover the cost of medications, take time off to recover, and pay for incidentals like transportation, parking and accommodations that can all quickly add up as out-of-pocket expenses.
Student debt
Paying for education creates unique financial stressors, including concerns about future earning potential, career choices, and delayed milestones such as marriage or home ownership. Student loans can contribute to feelings of pressure and affect overall well-being and the ability to focus and influence priorities when making financial decisions. Many students accumulate credit card debt on top of student loans to try and keep themselves afloat. Hiding from the situation can introduce mental health problems as students feel shame about being in debt and try to avoid adding financial stress to the academic stressors they are already experiencing. Experts agree that it’s essential for students to “get real about the debt they are taking on” as they often underestimate the length of time it can take to reduce or eliminate it. (3)
Emotional spending, instant gratification, and other influences
Emotional spending often comes from a desire for instant gratification, where we seek immediate pleasure through impulsive purchases. Societal, cultural, and parental influences can all play a role in shaping our financial behaviours. We receive messages about idealized success formulas that prescribe life milestones such as education, a stable job, marriage, home ownership and starting a family. It can be added complication as we break down and distinguish between good debt where we are investing in ourselves (like school or a mortgage) and receiving a payoff longer term, and bad debt (like high-interest consumer debt) which is more fleeting.
Individualistic versus collective cultures
Individualist cultures emphasize personal achievements and security independence, which may contribute to willingness to take on debt to attain personal goals. In contrast, collective cultures prioritize the community’s well-being, influencing financial decisions to align more with family expectations. Both situations can further complicate the psychology of debt.
What options and strategies are available to reduce and eventually eliminate debt?
Reducing and eliminating debt requires a comprehensive approach combining both practical strategies and a mindset shift. The key to managing debt is focusing on what you can control: developing habits, learning, and committing to making well-informed financial decisions. Here are ten options that you can explore:
-
- Create a detailed budget that outlines your income, fixed expenses, and other spending. Get insight into where your money is going so you can prioritize expenses and identify areas where you can cut back.
- Consider using a debt repayment strategy, such as paying off your smallest debts first or focusing on debts with the highest interest rates. Choose methods that will give you some traction in changing your financial situation and creating positive psychological gains.
- Build up even a modest emergency fund so that you have a bit of a financial cushion to fall back on during challenging times and avoid accumulating additional debt from unexpected expenses.
- Limit digital payments, especially credit card use. Set a monthly budget for discretionary spending and use only cash or debit for daily expenses to help control expenses. Establish separate accounts that align with budget categories so that you know where you are in your budget planning, stay on track, and don’t inadvertently overspend. Credit cards should be limited and reserved for specific expense categories only, such as essential travel.
- Evaluate credit products to increase awareness of incentives that encourage and influence overspending to earn rewards. Only choose those that align with your spending habits and financial goals. The alleged benefits may come at a significant cost in the longer term.
- Get assistance from credit counselling services, who can provide advice on budgeting, help develop debt management plans, and negotiate with creditors. These organizations can offer guidance about realistic debt repayment plans.
- Negotiate when you are struggling to make payments to see if your creditors have hardship programs available, can offer lower interest rates, or agree to a modified payment plan. Many are willing to work with people who are facing financial difficulties.
- Stay motivated by setting milestones for your debt reduction project. Breaking things down into smaller, achievable goals will help you see your progress and encourage you to keep going. Remember to celebrate each small success to change your mindset and improve your mental health.
- Improve your financial literacy by learning about the principles of personal finance. With this education, you’ll develop more confidence, allowing you to make informed financial decisions and build habits you can sustain.
- Consider working with a financial advisor or planner to get personalized advice for managing debt, planning taxes, investing, and creating and securing long-term direction. There’s a misconception that it’s a service only for people with lots of money. Meeting an advisor can help you determine your priorities and reduce financial stress.
Managing stress from debt
We can fear being unable to meet financial obligations, receiving constant contact from creditors, and worrying about the effect debt will have on credit scores. While these stressors are daunting, we can manage them. It starts with developing greater awareness about the behaviour patterns we may turn to when feeling stressed.
Look out for:
-
- A tendency to shop online, being lured or attracted by advertising and clever ways that retailers try to convince people and make it easy to buy. One approach that may work for you is purchasing pre-paid gift cards to use on your online shopping account to avoid using credit cards. This may allow you to control your expenses better and stick to a budget.
- Subscription models, boxes, and add-on deals that look enticing may seem to offer good value on the initial shipment, but often, the contract terms make it difficult to discontinue. Many people don’t end up using all the products shipped to them.
- “Experts” who promise quick and easy ways for you to make large sums of money with a small investment of time to attend a “free” online session that will provide you with all the training you need. These often try to allure you with the promise of earning more than you ever imagined was possible, allowing you to do what you want, when you want, working only a few hours a week. Often, there are significant buy-ins to participate in these programs that are disclosed in the introductory sessions. They can be legitimate businesses, but you must be aware that they are often built on multi-level marketing (MLM) models that present challenges.
- Online gambling that entices people to sign up for their services with a “free” incentive in a digital wallet can deepen debt and create setbacks and new burdens. These platforms are easy to access and present an increased risk of developing gambling addiction. When in debt, we can be desperate to make a gain and prioritize gambling over our financial responsibilities.
Take control by:
-
- Talking about your situation with someone you trust.
- Commit to taking care of yourself by recognizing that self-care can look like saying “no” to a wrong financial decision just as much as it can look like setting small, achievable goals.
- Seek professional help for debt-related stress. Your mind and body will thank you.
When you face debt and get support through financial counselling, therapy, or other resources, you will learn how to develop healthier financial habits. Prioritizing debt repayment and shifting your relationship with your finances will help you create a greater sense of responsibility and deliver the added benefit of feeling more in control of your physical and mental health.
References:
1. Munster, R. (2023 April 8). How Understanding the Psychology of Spending Can Improve Your Financial Well-Being. MoneyFit, by Debt Reduction Services (DRS). Retrieved November 6, 2023 from https://www.moneyfit.org/psychology-of-debt-unders…
2. Consumer Affairs Research Team, Edited by McCants, Cassidy (2023 June 1). Comparing the costs of generations. Consumer Affairs. Retrieved November 6, 2023 from https://www.consumeraffairs.com/finance/comparing-…
3. Novotney, A. (2013 January). Facing up to debt. American Psychological Association. Retrieved November 6, 2023 from https://www.apa.org/gradpsych/2013/01/debt
Linking Exercise and Nutrition to a Healthy Mind
Linking Exercise and Nutrition to a Healthy Mind

We have heard it before, eating well and regular exercise are important factors in maintaining a healthy body, but what do those actions mean for your mental health?
Mental health disorder research findings suggest that between ten and thirty percent of adults suffer from mood disorders, such as depression and anxiety. As a result of these disorders becoming more commonly diagnosed, physicians have been looking for natural methods to support their patients in treatment of mental health without medication. What the research is beginning to show is that people who suffer from depression or anxiety may improve their overall mental health through a balanced diet and regular exercise.
Exercise improves mental health
Physical exercise is increasingly being advocated as a means of maintaining and enhancing positive mental health. Findings suggest that getting twenty to forty minutes of aerobic activity can result in a reduction of anxiety for several hours.
Exercise tips to improve mind and body:
Getting started can be difficult, so start with small, manageable increments of physical activity and then slowly build to regular, more frequent exercise sessions. Setting exercise goals and being active for one day a week can begin your transformation of mind and body. If physical activity is difficult for you, using distraction methods such as listening to music or working out with a friend can help you develop a regular routine.
The benefits of jogging: Aside from the obvious physical health benefits, jogging for 30 minutes can also help with reducing stress, building confidence, improving focus, memory and overall attitude. Jogging once a week begins transforming the mind and body through positive endorphins which can result in one wanting to do it even more.
Walking at work: Making time to exercise can sometimes be difficult, so why not start with little steps throughout the workday to increase your physical activity. Try parking further from the door, taking the stairs, or having your lunch or meeting on the go. Make yourself accountable by challenging a friend or co-worker to do the same. Give yourself an extra challenge by adding ankle weights, helping to build your muscles and stamina.
Make exercise fun: Finding out what physical activity you enjoy is important to your journey of increasing physical activity. From gardening, to hiking, to yoga or even a simple walk around the block, there are several ways one can become more active. Tracking activity through fitness apps can help build a routine of physical activity and allow you to continue to challenge yourself.
Getting started can be difficult, so start with small, manageable increments of physical activity and then slowly build to regular, more frequent exercise sessions. Setting exercise goals and being active for one day a week can begin your transformation of mind and body.
Results of exercise and how it will help you:
As we have discussed various methods of getting active to improve your mental health, here are some of the health benefits from regular exercise you will begin to experience:
- Improved sleep
- Stress relief
- Improvement in mood and disposition
- Increased energy and stamina
- Reduced fatigue that can impair mental awareness
- Weight reduction
- Reduced cholesterol and improved cardiovascular fitness
When beginning your journey of increasing your physical activity, remember to be patient with yourself; it takes time to get into the habit of exercising regularly. Realise that any small step taken to increase your level of physical activity is better than not doing anything at all.
What you eat is what you feel
Trying to eat healthy when we are feeling low can be challenging, especially since typical comfort foods don’t tend to be the most nutritious. We often try to eat well for our physical health, but research suggests that healthy eating also plays a key role in mental health. When we don’t eat enough nutrient-rich foods, our body lacks vital vitamins and minerals, often affecting our energy and brain function. When certain nutrients are lacking in the diet, mood disorders, like depression, are more common. So, while it may be tempting to turn to a sweet treat for a mood boost, focusing on nourishing foods is much more likely to give you an emotional lift without the fall.
Here are a few tips on key nutrients to fuel your mind and body:
The power of protein: Protein is often praised for building muscle, but the role of protein goes far beyond the gym. Proteins are made up of amino acids; the precursors of neurotransmitters, which chemically transmit information from one nerve cell to another. Neurotransmitters increase levels of alertness and energy, while certain neurotransmitters like serotonin, dopamine, and norepinephrine are especially important for mental health. Protein rich foods contribute to improved cognitive functioning and well-being by increasing the quantity of neurotransmitters available in the brain. Fish, poultry, meat, eggs, nuts, seeds, lentils and beans are excellent sources of protein.
B vitamins for vitality: Dark leafy greens such as kale and spinach, citrus fruits, fortified breakfast cereals and beans are rich in Folate, a B vitaminoften deficient in people with depressive symptoms. Folate deficiency can cause serotonin levels in the brain to decrease, a key neurotransmitter which regulates our moods and how we feel. Sardines, salmon and eggs are excellent sources of this vitamin.
Get your omega-3 fatty acids: Essential fatty acids can alter the composition of nerve cell membranes. In fact, some studies have suggested that 250-500 mg per day of omega 3 fats may reduce symptoms of depression in some individuals, though the evidence is not conclusive. Instead of reaching for supplements, which may not be right for everyone, enjoy omega-3 rich fish such as salmon, mackerel, trout, or sardines at least twice a week. And what’s even better – these foods are also an excellent source of protein, calcium, and Vitamin D.
Enrich your diet with magnesium: Magnesium is required for over 300 separate biochemical pathways, such as the metabolism of energy and the production of protein. This important mineral also activates the enzymes needed for serotonin, dopamine and norepinephrine production which, if deficient, can cause symptoms of depression. Food sources for magnesium include nuts and seeds, dark green vegetables such as spinach, whole grains such as brown rice and bran.
Get a good source of selenium: Another mineral that can affect mood, selenium plays a key role in thyroid function. A healthy thyroid supports positive mental health which could reduce the risk of depression. Food sources of selenium include Brazil nuts, fish, shrimp, liver and chicken.
Before making changes to your exercise regimen or diet you should consult with your doctor.
The Role of Occupational Therapy in Mental Health Treatment
The Role of Occupational Therapy in Mental Health Treatment

In 2022, more than five million people in Canada met the diagnostic criteria for a mood, anxiety, or substance-use disorder, which amounts to about 13% of the population. For many, poor mental health is a barrier to living a full and productive life. Occupational therapy is a mental health treatment that can help them learn to adapt and participate more fully in the activities that give their lives stability, purpose, and joy.
Repairing connections to daily life 
Mental illness impacts every aspect of a person’s life, including their ability to participate fully in social, recreational, and employment activities. People who face mental health challenges can find themselves unable to work, attend school, or even enjoy activities such as hobbies or sports. As a result, their world becomes smaller and they become more isolated as their connections with the outside world are broken.
Among employed Canadians, 7.5% said they had taken time off from their job or business because of stress or for mental health reasons in the 12 months before April 2023. Every week, about 500,000 Canadians are unable to work due to poor mental health, resulting in 16% of working hours being lost to absences and presenteeism due to mental health issues.
Being unable to work has consequences that go beyond financial uncertainty. Work is a fundamental aspect of our identity and role within society. It gives structure to our lives, provides us with a sense of purpose and belonging, and brings us the respect of our peers.
The same is true of school, and similarly, the ability to attend school regularly is often interrupted by mental illness. A 2017 Ipsos survey of Ontario youth found that 46% of students surveyed reported missing school because of anxiety. And when they do attend, they don’t see as much benefit from the experience: children with poor mental health are 3.5 times likelier to have average grades of C or lower, and 25 times likelier to experience difficulty making friends.
Occupational therapy and mental health
Occupational therapy is used in many contexts, and occupational therapists can be found in a variety of settings. In a school, you may find them helping children develop skills and behaviours that will help them thrive in an academic setting. In a hospital, they can be found helping people with cognitive or physical limitations re-learn specific tasks or find new ways of doing things so that they can regain independence. In a mental health and addiction treatment centre, occupational therapists help people with depression, anxiety, post-traumatic stress disorder (PTSD), addiction, and co-occurring disorders to manage their conditions and regain their ability to take part in the everyday activities that make up daily life.
While physicians and psychiatrists make diagnoses, prescribe medication, and create individual treatment programs, occupational therapists help people with mental health conditions learn new ways of participating in work, school, and leisure activities by regaining or acquiring new skills, and adapting their environment (or their response to it) in ways that make it easier for them to participate in various activities.
 Part of an integrated mental health treatment
Part of an integrated mental health treatment
Mental health treatment requires a holistic approach that supports the whole person, including physical, mental, emotional, social, cultural, and spiritual components. Occupational therapists work closely with other practitioners and specialists to form a collaborative team that delivers holistic care.
This team can include physicians, psychiatrists, physiotherapists, prime therapists, nursing staff, addiction specialists, registered dieticians, recreational therapists, music therapists, art therapists, and horticultural therapists.
The role of the occupational therapist is unique in that it overlaps with and complements many other disciplines. In the context of mental health treatment, occupational therapy focuses on how the patient’s mental state—their thoughts and emotions as well as the symptoms of mental illness, such as fatigue, loss of motivation and meaning, fearfulness and hypervigilance—are preventing them from participating fully in every aspect of a balanced life.
How occupational therapy aids in mental health treatment
At Ravensview, a private mental health and addiction treatment centre on Vancouver Island, British Columbia, the occupational therapist uses a range of evidence-based approaches to support their patients in returning confidently to day-to-day life. These approaches can include:
Cognitive restructuring techniques: These therapeutic techniques help people recognize, challenge, and change negative thinking patterns that can become limiting and self-defeating.
Problem-solving skills training: This intervention gives patients the tools they need to identify problems and find ways to solve or adapt to them.
Activity exposure: Within an inpatient setting, occupational therapists help the patient build confidence by giving them a safe, controlled way to acclimatize to the environment and activity that they need or want to return to.
Supportive structure: Occupational therapists often help patients to create daily routines and set specific goals that help them progress along a path toward the desired lifestyle.
Motivational interviewing: Through empathetic, person-centred counselling, occupational therapists explore and resolve ambivalence, build personal motivation, and develop a plan for behavioural change.
During the treatment, the occupational therapist identifies medical and non-medical issues that are impacting the patient’s capacity, helps the patient improve their ability to identify and manage those issues, and supports the patient in strengthening their motivation for returning to work, school, or social and leisure activities.
The impact of occupational therapy
Effective mental health treatment takes a multidimensional view of a person’s life, including work, school, recreation, hobbies, and human interaction. By helping patients reconnect with these dimensions, occupational therapy can play a significant role in a patient’s recovery.
Including occupational therapy in a patient’s treatment journey can help to break a vicious cycle, where a person with mental illness withdraws from work, school, exercise, leisure, and social activities, which in turn puts them at greater risk of poor mental health. In fact, this type of therapy can help to accelerate recovery by creating a “flywheel” effect, where the return to fulfilling activities helps to accelerate the patient’s return to health through participation in meaningful and beneficial activities.
Occupational therapy helps people with mental health issues achieve a number of crucial recovery milestones:
Increase physical movement. The link between exercise and mental health has been extensively researched and confirmed. Evidence from a meta-analysis of 49 studies spanning 260,000 participants shows that people with higher physical activity levels are less likely to develop depression, which is why recreational therapy also plays an integral role in mental health treatment.
Get back to work. The inability to perform work has financial and psychological consequences, resulting in a loss of self-esteem, work relationships, structure, and purpose. A meta-analysis found that 14 of 16 longitudinal studies on the impact of unemployment and mental health showed a significant, negative association. By helping people return to gainful, meaningful employment, occupational therapy improves their mental health.
Create social connections. Depression, anxiety and cognitive decline (in older people) are all associated with social isolation and having fewer social ties. Research from Statistics Canada showed that 62% of socially connected people with mental health-related disabilities rated their mental health positively compared to only 49% of those who were not socially connected.
Enjoy hobbies. Research shows that having a hobby is linked to lower levels of depression – and may even prevent depression for some people—even those who have clinical depression. Spending time outside in nature has also been shown to have a protective effect on mental health, as do creative pastimes such as music and art.
We are what we do
For most of us, what we do on a daily basis defines us and gives us our sense of identity and self-worth, whether it’s the contribution we make to the world through our work or the things we do in our down-time that bring us joy. When we experience a mental illness, we often lose those essential parts of ourselves. Occupational therapists help patients find ways of regaining them so that they can participate in and benefit from a return to normal, daily life.
National Ride for Mental Health
National Ride for Mental Health

Check out this video recap of the National Ride for Mental Health held in August!
From Victoria to Guelph to Ottawa, we rode, as a National Partner, in support of Wounded Warriors Canada and raised over $40,000.
Thank you to everyone involved. We hope to see you next year!

Breaking the Silence – Navigating Men’s Mental Health Challenges and Offering Support
Breaking the Silence – Navigating Men’s Mental Health Challenges and Offering Support

There are many stereotypes of masculinity. Men are supposed to be strong and emotionally resilient, but these persistent ideals have shaped expectations placed upon men for too long. Instead, they’ve fostered a culture that tends to discourage men from expressing their vulnerability and emotions because “real men” should be stoic and unyielding. All of this directly affects men’s mental health; breaking the silence around it is a pressing imperative.
Societal and cultural influences perpetuate the myth that men seeking help for mental health struggles are weak. These ingrained beliefs have profound consequences and contribute to the alarming rates of undiagnosed and untreated mental health issues among men. It is time to recognize the need to dismantle barriers and foster an environment where men feel both empowered and encouraged to be open about their mental health. Ultimately, achieving this will pave the way for happier and healthier lives for everyone.
In this article, we’ll address the complexities of men’s mental health. We can start to break free from some of the constraints of societal and cultural influences and relieve some of the pressure that men experience that influences their reluctance and delay in seeking help for mental health. Talking about men’s mental health transparently is essential to reduce stigma. It also emphasizes the need for everyone to recognize how there is more room to be more compassionate.
How does stigma affect how men relate to mental health challenges?
Despite advances and improvements in our overall understanding of mental health, men experiencing mental health challenges often suffer alone. Stigma creates additional complexity when people struggle because they often experience “discrimination, avoidance, and rejection.” (1) It has many facets, including “social (public) stigma, self-stigma (perceived), professional stigma, and cultural stigma,” which create “extreme barrier[s]” for seeking help.(2) Many men fear being seen as less masculine or weak, which can build feelings of inadequacy and worsen their self-esteem. Stigma can influence men’s choices towards less healthy coping mechanisms like aggression or substance use to help them deal with emotional pain. Some men tend to be more comfortable focusing on physical ailments instead, which in turn delays diagnosis and treatment and creates longer recovery times.(3)
From an early age, social conditioning encourages boys to be “strong, independent and emotionally stoic, while girls are expected to be nurturing, empathetic, and compliant.”(4) The long-term effects have men “hide their vulnerabilities and suppress their emotions”.(5)
What are some notable differences in men’s mental health experiences?
The mental health challenges men experience are likely far more common than reported. For example, while depression can affect anyone, regardless of gender, there are differences in how men and women experience and exhibit symptoms. Some researchers have observed that men have more difficulty processing loss and grief over their lifetime. Many life stressors, such as physical illness, financial problems, and relationship breakdowns, become overwhelming and contribute to the manifestation of grief. (6)
Here are some differences to be aware of in how depression may present differently in men and women.
How does this information apply when people identify as Transgender, Gender Neutral/Non-Binary?
It’s critical to approach mental health with an open mind that considers gender-affirming and inclusive perspectives, recognizing that someone’s biological and psychosocial influences can vary widely and may not align with traditional expressions of symptoms of mental health challenges or distress.
- They may have coping mechanisms that depend on their unique identity and experiences and do not align with traditional gender roles.
- If they experience gender dysphoria, they feel more intense distress and depression.
- Their gender identity may influence access to mental health care and supportive services. It can affect their ability to access gender-affirming appropriate treatment. It could “create a profound sense of isolation, as they may feel misunderstood or rejected by their communities.” (9)
- They may experience chronic stress due to “fear of judgement, discrimination, or violence.” (10)
Mental health professionals need to be sensitive to the specific needs and tailor therapy that acknowledges the impact of gender identity as part of the assistance.
What do studies tell us about how prevalent mental health issues are for men?
The statistics about men’s mental health can be shocking, but being well-informed can help increase awareness of how crucial it is to change the narrative and encourage men to get the help they need.
- In the U.S., over 6 million men suffer from depression yearly. It is often underdiagnosed. (11)
- More than 3 million men in the U.S. have panic disorder, agoraphobia, or another phobia (12)
- 90% of the 3.5 million people in the U.S. who live with schizophrenia are men, diagnosed by age 30. (13)
- The highest suicide rates in the U.S. are in Caucasian men over 85. (14)
- In the U.S., gay males are at an increased risk for suicide attempts, especially before age 25. (15)
- While approximately 1 million Canadian men suffer from major depression yearly, only 30% use available mental health services. (16)
- 80% of Canadian men have spoken with a healthcare practitioner in the past 12 months as of June 2023. (17)
- Canadians were more likely to prioritize their physical health than their mental health. However, while nearly 1/3 of women selected mental health as a top priority, only ¼ of men noted the same. (18)
- 26% of Canadian men said that if they were feeling down or agitated more often than usual, they would either wait over a year or not make an appointment at all if these feelings arose. (19)
- 76% of all suicides in Canada in 2019 were by men. 38% (the highest number) were men aged 40-60. (20)
- While women attempt suicide twice as often as men, men die by suicide three times as often as women. (21)
Suicide disparities for men
Men consistently have higher suicide rates in many countries worldwide, especially in middle-aged and older age groups. They also tend to use more lethal methods that are more likely to have their attempts result in death. Targeting mental health awareness is crucial to help reduce the stigma surrounding seeking treatment for mental health challenges. At the same time, the available services must be accessible and gender sensitive. Family, workplace, and community support are essential in suicide prevention.
What are some beneficial prevention and intervention strategies?
Remember that a combination of strategies may be most effective, recognizing each person’s individual needs and circumstances.
Increasing awareness and accessibility when it comes to men’s mental health, services can work to avoid glamorizing or sensationalizing suicide through more responsible portrayals of men in the media who are dealing with mental health issues. It can also encourage more men to be open to conversations within their communities, families, and workplaces. Education can help us to:
- Recognize signs of mental health distress and promote help-seeking to destigmatize the issue.
- Ensure that access to mental health and crisis supports are available, accessible, and affordable.
- Train first responders, community leaders, teachers and medical teams to recognize men’s unique warning signs and specific risk factors such as excessive or untypical substance use or aggressive behaviour.
- Be open to developing support networks, social connections and self-help resources tailored to men’s needs and introduce the value of help-seeking and positive coping strategies to build resilience.
- Create crisis intervention plans for men who are at risk that outline what steps to take in case of a mental health emergency.
- Restrict access to weapons/firearms, medication, and other lethal means that men tend to access during crises.
Stress reduction techniques and healthy coping mechanisms can help men understand how to detect vulnerable changes in their mental health status rather than waiting for a crisis. For example, there are proven benefits of regular exercise in that it can:
- Reduce stress, anxiety, and depression.
- Improve a sense of self, boosting mood, self-worth, and self-esteem.
- Boost energy and clarity of thinking.
- Help release beneficial endorphins to clear the body of stress hormones such as cortisol.
- Be beneficial to participate in collaborative sports teams and avoid ultra-competitive/individualistic sports that build machoism.
Not discounting the value of self-care basics and engaging in enjoyable activities can also prevent crises. It may include quite apparent things but also help with releasing inhibitions that may be holding someone back:
- Getting restful sleep.
- Practicing good nutrition.
- Finding purpose through friends, family, and community involvement to forge social connections and belonging.
- Speaking with a therapist to explore supports/boundaries and develop resilience. It could also involve joining a peer support group for other men experiencing similar feelings or fulfilling similar roles and obligations.
Encouraging conversations about men’s mental health
Common stereotypes that hinder open discussions about men’s mental health include:
- The expectation that men should not show emotions, express vulnerability, or ask for help.
- The belief that men should be tough, aggressive, and dominant.
- The idea that men must be independent and self-reliant to solve all problems on their own without seeking support or help.
- The fear that admitting to mental health struggles will be seen as a weakness, failure, inadequacy, or somehow less masculine.
- The tendency to suppress strong emotions and feelings rather than address them earlier and be more proactive in looking for solutions to pain and promote recovery.
- The insensitivity of common expressions such as “man up” that trivialize normal emotional responses and promote vocabulary limitations that suppress emotional expression.
- The fear of being judged by peers, co-workers, partners, or family members if they are transparent about their mental health.
Breaking these stereotypes down helps create a supportive environment to address men’s mental health needs without fear, stigma, or judgment. We must provide safe spaces for men to discuss their feelings and share their experiences openly.
Conversation Starters
While it can be difficult for men and others, starting with an open conversation can be the best approach to take. Consider trying some of these suggestions to start a conversation if you notice someone in your life may be struggling: (22)
- How are you feeling on a scale of 1 to 10?
- You’ve been a bit quiet, how are you?
- How is work at the moment?
- When did you start feeling this way?
- How are you coping?
- Who else can you talk to?
- What help do you need?
The power of education and awareness
Some prominent men have overcome stigma and sought help, demonstrating that to do so is a sign of strength. Their stories can encourage other men to do the same.
- 1. Prince Harry has been candid about struggling with grief and mental health after his mother’s death. He co-founded the Invictus Games to promote open conversations about mental well-being and camaraderie for military service people through sport.
- 2. Comedian Trevor Noah has spoken publicly about his experiences with depression to challenge mental health stigma and promote understanding.
- 3. Actor and comedian Wayne Brady has shared his struggles with depression and anxiety to encourage other men to seek help and prioritize mental health and well-being.
- 4. Actor and former wrestler Dwayne “The Rock” Johnson has openly discussed his struggles with depression and advocates for increased mental health awareness and self-care.
We’re also sharing some resources published by the Centre for Suicide Prevention and Mental Health that you can explore. They have been specifically developed for men. (23)
Buddy Up – A men’s suicide prevention communications campaign: a call to action to men, by men
Tough Enough to Talk About It – A program for men working in trades, industry, and agriculture
Man Therapy – An interactive website that encourages men to address their mental health and seek help if necessary
DUDES Clubs – Spaces that facilitate a participant-led community for men’s wellness
HeadsUpGuys – Online information and resources to encourage help among men at risk for depression and suicide
Men’s Sheds – Community-based safe and friendly environments where men can learn practical skills, develop new interests, work on meaningful projects, connect with other men, and talk about their problems
Movember – Information about mental health and suicide prevention
Men’s mental health is not just about individual well-being. It benefits us all by creating a more inclusive, empathetic, and supportive environment. By dismantling stereotypes around men’s emotional well-being, we can help save lives, improve relationships, and promote gender equality. Supportive changes in perception will help break the silence around men’s mental health.
References:
1. Chatmon, Benita, PhD, MSN, RN, CNE. (2020 August 19). Males and Mental Health Stigma. American Journal of Men’s Health. Retrieved August 29, 2023 from ttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC7444121/
2. Ibid.
3. Duran, Andres, LPCC. (n.d.) How Mental health Stigma Impacts Men. Sage Neuroscience Centre. Retrieved August 29, 2023 from https://sageclinic.org/blog/stigma-impacts-men/
4. Hodge, Kayne. (2023, June 16). Gender Roles and Their Impact on Depression: Beyond the Surface.Mental Health Centre. Retrieved August 29, 2023 from https://www.mentalhealthcenter.org/gender-roles-an…
5. Ibid.
6. Ogrodniczuk, J. PhD. & Oliffe, J. PhD. (2011 February). Men and depression. Canadian Family Physician. Retrieved August 29, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC30388…
7. Ogrodniczuk, J. PhD. & Oliffe, J. PhD. (2011 February). Men and depression. Canadian Family Physician. Retrieved August 29, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC30388…
8. Ibid.
9. Hodge, Kayne. (2023, June 16). Gender Roles and Their Impact on Depression: Beyond the Surface.Mental Health Centre. Retrieved August 29, 2023 from https://www.mentalhealthcenter.org/gender-roles-an…
10. Ibid.
11. Mental Health America, as cited in Anxiety & Depression Association of America (ADAA) (n.d). Men’s Mental Health: Why Men’s Mental Health is Important. ADAA. Retrieved August 29, 2023 from https://adaa.org/find-help/by-demographics/mens-me…
12. Ibid.
13. Ibid.
14. Mental Health America (n.d.) Infographic: Mental Health for Men. Retrieved August 29, 2023 from https://www.mhanational.org/infographic-mental-hea…
15. Ibid.
16. Parent, A. (2023 January 26). Mental health and men: how to support your loved onesI. Canadian Red Cross Blog. Retrieved August 29, 2023 from https://www.redcross.ca/blog/2023/1/mental-health-…
17. Movember Canada as cited in CISION (2023, June 12). New Survey Suggests Positive Shift: Shows Men More Proactive in Managing their Physical Health, Continue to Struggle Prioritizing Mental Wellness. Retrieved August 29, 2023 from https://www.newswire.ca/news-releases/new-survey-s…
18. Ibid.
19. Ibid.
20. Centre for Suicide Prevention and Mental Health Commission of Canada (2022 March 30). Men and suicide. Retrieved August 29, 2023 from https://www.suicideinfo.ca/local_resource/men-and-…
21. Ibid.
22. Mental Health Innovations (n.d.) Talking about men’s mental health: conversation tips. Men’s Health Innovations Charity. Retrieved August 29, 2023 from https://giveusashout.org/latest/talking-about-mens…
23. Ibid.
Suicide Prevention: Uncovering the Signs
Suicide Prevention: Uncovering the Signs

During these unprecedented times of COVID-19, the importance of mental health and our overall well-being has received more attention than normal. Throughout the pandemic, people have felt the overwhelming sense of loneliness, isolation and experienced multiple disruptions in their daily routine. The added economic concern, with realized job loss or threat thereof, has layered new realities and complexity to our individual and collective mental health. Although not necessarily the primary cause for one to consider ending their life, COVID-19 has become a contributing factor that influences one’s decision to consider suicide.
On average, we’re spending more than a third if not half of our waking hours at work. Colleagues often become friends rather than just colleagues and will offer you glimpses of their inner lives. Suicidal thoughts and plans are the last thing you would expect to be shared. However, what if you become aware that a colleague is contemplating suicide?
In this article, we’ll be looking at:
- What are the predisposing and contributing factors of suicide
- What are potential signs of suicidal risk in a co-worker
- How to provide support while respecting confidentiality and safety issues
- How to promote self-care and seek outside support if needed
But first, some facts…
For every death by suicide there are 20 to 25 attempts, 5 self-inflicting injury hospitalizations and 7 to 10 people deeply affected by grief.
On average, suicides claim the lives of 12 Canadians per day. In 2015, 3,269 Canadian men and 1,136 women died by suicide. (1) However, women make up to 3 to 4 times more suicide attempts than men. The actual suicide rate for women has risen by as much as 50% from 2000 to 2016 in the U.S. (2) and a similar trend has also been observed in Canada. Overall, the prevalence of suicide is growing. According to Fardous Hosseiny, the national director of research and public policy at the Canadian Mental Health Association, the percentage change over 2011 and 2015 shows an increase of 12% in males and 15% for women. The largest population of suicides in Canada are from working aged men and women between the ages of 30 to 64 with a peak occurring between 45 and 59. (3) The suicide rate among the U.S. working-age population increased by 34% between 2000 and 2016. (4)
Workplace suicides have also increased. Approximately 1,719 male and female workers ended their lives on the job in the U.S. between 2003 and 2007. (5) In 2016, the American Bureau of Labor Statistics reported a steady increase in workplace suicides from 2007 to 2013. In 2018, the Mental Health Commission of Canada published a study that found Canadian employees reported workplace stress as the primary cause of their mental-health concerns. (6) Steve Bittle, an associate criminology professor at the University of Ottawa states that between 10 and 17 per cent of annual suicides in Canada could be classified as work-related, representing a range of 400 to 800 fatalities each year. (7)
In November 2018, the CDC (Centers for Disease Control and Prevention) reported that the top 3 major occupational groups by suicide rate among males in 2015 were:
- Construction and Extraction
- Arts, Design, Entertainment, Sports and Media
- Installation, Maintenance, and Repair
For women:
- Arts, Design, Entertainment, Sports and Media
- Protective Service
- Healthcare Support
For both genders, the lowest suicide rates in 2015 were observed in education, training and library occupations.
In general, occupations with higher suicide rates involve one or many of the following factors: easy access to lethal means, exposure to chemicals, high workplace stress and risk of trauma, job insecurity, low wages, inconsistent work schedule and isolation in the workplace.
Rising workplace suicide rates shouldn’t come as a surprise in an era crippled with progressively increasing levels of pressure and stress among employees. Now the added complexity of COVID-19 has created new factors that influence the rising statistics. According to the HR Digest, the obsessive focus “on targets and deadlines, race for profits and excessive individualization as well as informal competition amongst colleagues are some of the causes of suicidal tendencies. They lead to psychological problems in the workplace which have a negative impact on the way employees work.”
When a suicide does occur, work and/or business related colleagues can be emotionally impacted with feelings ranging from anger, grief and guilt. These feelings can last far beyond the initial shock and reaction time span. Feelings and reactions may also surface within colleagues who weren’t close to the employee who took their own life. Often, death by suicide leads to rumors and speculation about why it took place. These rumours may include work-related factors and could potentially affect the morale of employees.
Predisposing and Contributing Factors
Causes for suicide are a complex cocktail of factors, including relationship breakdowns, financial difficulties, chronic physical illness, major losses, major social disruptions or a lack of social support. Some factors can be work and career related. It has been found that for every 1% increase in unemployment, there is a 0.79% increase in the suicide rate. (8) During the Great Depression, the suicide rate in America increased by 21%.
A common predisposition is an underlying mental health disorder, as 60% of completed suicides involve people dealing with a diagnosed depression. Moreover, 90% of people who take their own lives suffer from a mental health disorder. (9)
When professionals estimate the risk of suicide among employees, they will take into consideration some of the following predisposing factors:
- Access to lethal weapons
- Past suicide attempts
- Capacity to hope for positive change
- Self-help capacity, including diet, quality of sleep, medication and professional follow up
- Chronic mental health suffering and/or physical pain
- Self-control and impulsivity
- Substance usage and/or abuse
- Support network, which serves as a protective factor.
Uncovering the Signs
Depending on how close you are to a co-worker, you may or may not know of the above predisposing factors but some signs can give you hints as to the potential risk of suicidal thoughts or plans. None of these, on their own, can reveal suicidal risk, but a combination of some of the following signs can reveal a significant level of distress within your co-worker. About 75% of those who die by suicide do exhibit some suicide warning signs. 10
Work-related signs or situations to look for are isolation, performance and stress-related anxiety, conflicts with management or colleagues, job insecurity, intense expressions of job dissatisfaction, deep and long-lasting fatigue, workload issues, and presenteeism or absenteeism. It’s important to recognize that some of the previous symptoms can also be traced back to personal problems affecting the well-being and mental health of a colleague. Mental health disorders influence feelings, thoughts, behaviour and abilities. Employees dealing with a disorder may show losses in confidence, concentration and patience. It might impair their decision making, judgement and people skills. Their personality can be altered and subject to mood swings and extreme shifts in behaviours and attitudes.
More typically linked to suicide are comments on being a burden to others who they say would be better off if they weren’t there; or employees becoming suddenly very happy after a depression or despite everything crumbling down around them. More obvious warning signs require more immediate action, such as someone expressing the desire to die or to end their life and having a plan to do so. (11)
It’s estimated that up to 25% of people do not exhibit signs before ending their lives. It’s important not to blame yourself or others if a colleague completes suicide without any visual or behavioural cues. However, if you recognize any of the signs mentioned earlier, don’t hesitate to engage in a conversation with your co-worker. If you happen to be right, starting that conversation might just save your colleague’s life.
How to Provide Support
If you approach a colleague you believe might be suicidal, tell them you’ve noticed changes in their behaviour. Be respectful and share your concerns. Ask if the person is okay. It’s normal to feel uneasy and it can indeed be scary. But asking someone about suicide doesn’t put the idea in their head. Instead, according to the Ontario Suicide Prevention Network (OASP):
- It breaks isolation which can distort their fears, hopelessness and embarrassment.
- It breaks the silence and sends a powerful message that they are not alone, that you care and that it’s okay to talk about their thoughts and feelings.
- Opening up a conversation about suicide is the first step towards hope and almost always helps reduce the risk.
- It lets people the opportunity to let their fear out and to consider and talk about other options. Suicide is often less about wanting to die, and more of a feeling or belief that they have run out of options.
Be cognizant of the individual’s right to privacy and never jump to conclusions. However when you genuinely believe there is a risk of suicidal thoughts or plans:
- Don’t hesitate to ask your colleague directly if they are having difficulties. If the answer is yes, ask if they have thoughts or plans of suicide.
- If they do have thoughts or plans of suicide, first acknowledge that this is serious. Don’t act right away. Keep the person talking and keep listening. This shows empathy and understanding. It creates the necessary bond you need to build before you even mention outside help.
- Foster hope by exploring potential options for help. Seek to find supportive people like professionals or important persons in their lives that are well suited to identify better options. Remember, the suicidal person is seeking a way out of a painful situation. They are often in the dark and have lost hope, shedding light on a different road map can help them to recognize and consider other pathways.
- Check on prior attempts. You can ask you colleague if they has tried to hurt themselves in the past. If they have, the risk of suicide increases making it more urgent to get professional help.
- After your conversation, don’t let this rest upon your shoulders. You can express your concern about needing to get help in order to keep your colleague safe. Refer them to resources in your workplace (HR, EFAP), or to a mental health professional or a community resource, like a crisis centre.
The person has to be put in contact with the chosen resource as soon as possible. It is important that a person entertaining thoughts of suicide be linked to a well-trained professional that can perform a comprehensive suicide assessment and intervention within the day. (12) In the meantime, make sure your colleague is not left alone. Either stay with your colleague or ask if they have a close friend or family member that can be with them. Be sure to let your colleague know, they need to tell someone and seek help if risk of harm exists.
Remember that security issues always outweigh confidentiality considerations if a person is deemed in danger of inflicting imminent harm to themselves in a way that can threaten their life or the life of others.
Self-care
Providing support to a suicidal colleague is not easy. It can affect you emotionally, put you in a state of constant worry and make you feel responsible for one’s well-being. Crisis and suicide prevention centres most often offer support services for people who are themselves a support to a suicidal person. Your EFAP and HR resources might also offer such services. Your personal network of family and friends is also an important resource, but go to a professional support system first. It will make you better informed and should lift much of the weight of responsibility off your shoulders.
If you would like more information on suicide alert programs or training to develop skills in suicide intervention, many local and provincial suicide prevention community resources offer training and even workplace gatekeeper programs.
A positive aspect of COVID-19, one’s mental health has become more accessible. Free to all Canadians, Homewood Health is a proud partner in Wellness Together Canada. This online portal offering free resources, tools and mental health support services in both English and French. It can be accessed at wellnesstogether.ca or by phone by calling 1-866-585-0445.
No one is immune from suicidal thoughts and urges. If such thoughts should invade your mind, don’t isolate yourself, talk to someone you trust and ask for professional help. You don’t have to suffer in silence.
No one is immune from suicidal thoughts and urges. If such thoughts should invade your mind, don’t isolate yourself, talk to someone you trust and ask for professional help. You don’t have to suffer in silence.
References:
1. Statistics Canada, 2015, as reported by Global News. Source : https://globalnews.ca/news/4274136/suicide-rates-w…
2. Dr. Hedegaard, H., Suicide Rates in the United States Continue to Increase. National Center for Health Statistics (NCHS). 2018. Source: https://www.cdc.gov/nchs/products/databriefs/db309…
3. Statistics Canada, 2015. Source : http://dustinkmacdonald.com/canadian-suicide-stati…
4. Suicide Increasing Among American Workers. Centers for Disease Control and Prevention (CDCP) press release. 2018. Source: https://www.cdc.gov/media/releases/2018/p1115-Suic…
5. American Bureau of Labor Statistics (ABLS). Source : https://www.thehrdigest.com/workplace-suicides-ris…
6. Canadian employees report workplace stress as primary cause of mental health concerns. Mental Health Commission of Canada. 2018. Source: https://www.mentalhealthcommission.ca/English/news…
7. Job-related deaths in Canada dramatically under-reported, study suggests. CBC News, January 29, 2019. Source: https://www.cbc.ca/news/canada/workplace-fatalitie…
8. Stuckler,D. et al. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. The Lancet. 2009. Source: https://www.thelancet.com/journals/lancet/article/…61124-7/fulltext
9. Public Health Agency of Canada, 2016. Source: https://www.canada.ca/en/public-health/services/pu…
10. Source : http://www.suicide.org/suicide-warning-signs.html
11. American Association of Suicidology, 2017. Source: https://www.suicidology.org/resources/warning-sign…
12. LivingWorks Canada, 2007. Source : http://www.ospn.ca/index.php/suicide-prevention/su…
Moral injury in healthcare and the role of self-care
Moral Injury in Healthcare and the Role of Self-care

The traumatic legacy of the pandemic continues to impact the mental health of Canadian healthcare workers who put their lives on the line. Practicing self-care can help them heal.
July 24 is Self-Care Day, a day to recognize the importance of self-care in empowering people to look after their own health. For healthcare professionals in Canada, it’s a day to explore the ways in which self-care can play a role in helping to manage the toll that this important work can take on their mental health.
Dr. Tara Riddell is a psychiatrist for the Addiction Medicine Program and the physician wellness lead at the Homewood Health Centre, a leading inpatient treatment facility in Guelph, Ontario, that focuses on mental health, trauma, and addiction. She began exploring the relationship between mental health and self-care early in her career.
“In medical school, I started my research with the goal of reducing stigma related to mental health amongst the general population,” she explained. “But I soon recognized that this was a significant issue for myself and my healthcare colleagues, who have high rates of burnout, depression, anxiety, and suicide risk. I began to think about how I could take care of myself throughout my career journey and what other healthcare professionals may need to feel well and fulfilled in the work that we’re doing.”
Stress management for healthcare professionals has always been a challenge, but when the pandemic struck, the situation rose to crisis levels.
 Moral injury: The pandemic legacy
Moral injury: The pandemic legacy
In 2020, psychological distress in healthcare began to make headlines. As healthcare professionals all over the world risked their lives to continue delivering care under trying circumstances, their mental health suffered, and the rates of moral injury soared.
Moral injury is a type of stress caused when a situation forces a person to behave in ways that go against their moral code. Its impact on mental health is profound, and it can result in depression, anxiety, and post-traumatic stress disorder (PTSD) for healthcare professionals.
According to data collected in 2022, Canadian healthcare providers were exposed to a host of morally injurious events during the pandemic, including watching their patients die alone, witnessing patient harm, being exposed to bullying and violence, not having access to adequate resources and personal protective equipment, and coping with increased workloads and decreased staffing. In one study, a staggering 81% of Canadian healthcare workers said they were exposed to an unethical culture, 55% said they were exposed to a low psychosocial safety climate, and 50% said the quality of care was hindered.
As a result, the rates of moral injury for healthcare professionals in Canada rose dramatically. An online survey of Canadian physicians conducted in 2020 found one-third of respondents had considered leaving or previously left a position because of moral distress and another one-third met the criteria for burnout syndrome. In another survey of Canadian healthcare workers conducted in 2022, 25% had considered leaving their profession due to moral distress, 25% met the criteria for PTSD, and 60% had significant levels of depression.
A resistance to self-care
Dr. Riddell is quick to stress that solving the issue of moral injury in Canadian healthcare requires systemic change, including more resources, a bigger workforce, and improving the coordination of care. But she is also a strong proponent of practicing personal self-care as a way to manage stress and prevent burnout and moral injury.
However, healthcare professionals have a tendency to resist this approach. “Healthcare is not a culture that has been compassionate to our own vulnerability or suffering or perceived weakness, or even the disclosure at work of mental health challenges or concerns,” she said. “Sometimes it can be very challenging for health care providers to engage in self care, because we feel guilty for it, or we feel it is selfish. But in order to be at your full capacity to help others, you need to take care of your own needs first.”
From shame to acceptance
Removing the stigma around mental health is a crucial part of the process. Ironically, healthcare workers who treat their own patients with tremendous understanding often feel shame around their own mental health issues.
But extending the same sense of compassion to ourselves that we extend to our patients is the foundation for effective self care. Dr. Riddell said that when we see the difficulties or challenges we experience as part of a shared human experience, it can reduce the stigma and break down barriers.
“It allows me to have more open conversations with colleagues about something that’s weighing on me and to recognize that I’m not any ‘less-than’ as a health care provider for having some of these challenges. It helps me shed some of the shame and do a little bit of internal healing.”
Healthcare Salute, a resource for healthcare professionals who may be experiencing or at risk of moral injury, provides a helpful mental health model to help people self-assess their mental health and determine the actions they can take to improve it. The model is also intended to reduce the stigma around mental health issues by placing the full range of experiences on a continuum.
The Mental Health Continuum
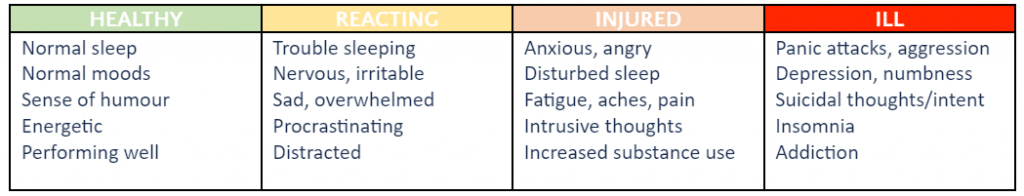
(This table is condensed and adapted from the Mental Health Continuum Model developed by Healthcare Salute. See the full continuum here.)
 Five ways to practice self-care
Five ways to practice self-care
Dr. Riddell believes that every healthcare professional can benefit from practicing self-care, no matter where they fall on the continuum of mental health.
“I often use the image of an internal tank,” she explained. “Through personal and especially professional responsibilities, our tank has lots of little drains. When our tank becomes depleted, we begin to experience greater challenges, and that’s where we may experience burnout or other mental health concerns. Self-care is a way to help refill our tank, or at the very least slow some of those drains.”
Dr. Riddell recommends these simple self-care tactics as a way for healthcare professionals to make small changes that can protect their mental health and replenish their internal tank.
Take ten. “I think everyone in healthcare has skipped a meal or a snack break or a bathroom break. Sometimes self-care means saying, ‘I may be late, but I need to take care of a basic need. If I take ten minutes to have a snack or lunch, I’m going to feel better and I’ll be able to be more present with the person I’m meeting with next.”
Try mindfulness. “In Homewood Health Centre’s Addiction Medicine Program, many of our healthcare providers incorporate mindfulness into their day. In times of heightened distress, they utilize deep breathing, attend to their own emotions, and practice ways of grounding themselves.”
Go offline. “My colleagues are increasingly finding ways to set limits on the work we do. I’m seeing staff identify when they’re going to be offline and indicate that they won’t be responding until a later date so that they have that protected time to recover.”
Reach out. “Social connection and engagement, especially with people who are also going through similar experiences, is an important way to foster self care. Social well being is one of the components of our wellness.”
Set priorities. “Increasingly, for all of us, time is a very scarce commodity. I try to think about how I’m using my time, and whether the things that are taking up my time are ultimately aligned with my core values. If they are, I’m more likely to feel a sense of enjoyment from doing it or a sense of fulfillment and meaning. And that helps me refill my tank.”
From “work warrior” to “wellness warrior”
People choose careers in healthcare because they want to nurture the health of others, but the soaring rates of moral injury for Canadian healthcare providers has shown that we’re not always as attentive to our own health. While self-care can’t mend a healthcare system in crisis, it can help those who work within it to protect their precious mental health.
“In our culture, we’ve often celebrated the work warrior, the person who is always taking on new challenges, never stops, and sacrifices their own needs,” Dr. Riddell pointed out. “Maybe we should be celebrating people who are prioritizing their wellness because they know that’s what they need and is going to be beneficial to their team and to patients.”
More self-care insights and ideas
An ongoing Canadian national study is now investigating the causes and impact of moral injury in Canadian healthcare professionals. The study involves a collaboration between Homewood Health, which has donated funds and expertise, the Homewood Research Institute, McMaster University’s Department of Health Sciences – Psychiatry and Behavioural Neurosciences, Atlas Institute for Veterans and Families, St. Joseph’s Healthcare, Western University, IDEaS, and the Public Health Agency of Canada.
As part of the project, Healthcare Salute was launched to share information, resources, and stories to help HCPs get the support they need to connect, self-assess, and practice self-care.


