Interconnections Between Stress, Diabetes, Nutrition, and Mental Health
Interconnections Between Stress, Diabetes, Nutrition, and Mental Health

Most people know that stress is something to reduce or avoid, but it may be surprising to learn how much it can affect our overall health and well-being. It’s especially true for people who are living with metabolic diseases like diabetes.
Stress significantly affects our body’s ability to stabilize blood sugar levels and reach a manageable state. What’s perhaps more problematic is that it’s thought that close to 40% of those with diabetes are unaware they have it. (1) When imbalanced and uncontrolled, diabetes can lead to various complications, including cardiovascular disease (stroke and heart disease), kidney problems and nerve damage.
This article will look at the interplay and relationships between stress, nutrition, diabetes, and mental health. With a better understanding of how everything is connected, we can explore some early warning signs that could make you want to determine your diabetic status. From there, we can share some tips to help you think about how stress might affect how your body processes glucose and determine how to reduce stress overall for better health.
How does stress affect blood sugar levels?
When stressed, cortisol and adrenaline are released into our bodies, prompting our pancreas to release stored glucose into our bloodstream. It’s a natural response: these hormones raise blood sugar to react to a fight-or-flight situation. This happens in a fraction of a second and starts a complex sequence of events. (2)
When our bodies perceive a threat, this instinctive reaction gives us the quick energy we might need to survive it. At the same time, we need to be able to lower blood sugar levels when we aren’t under threat to ensure that all our cells have the necessary energy to function correctly. Insulin is the chemical signal responsible for regulating glucose and determining how we store nutrients in our liver and muscles. It also plays a significant role in how our bodies hold fat molecules. Being in a state of chronic stress can lead our bodies to develop a state of chronic inflammation and is linked to a condition referred to as insulin resistance.
Chronic stress doesn’t allow for the natural conditions to have insulin work to clear away elevated levels of stress hormones within our bodies. Over time, cells become less responsive to insulin while it tries try to simply do its job as the natural chemical messenger it is. When that happens, our bodies pay less attention to those signals, and how we absorb and clear glucose in our bloodstream becomes impaired. Since insulin is such an essential energy regulator, improper functioning can affect our overall health in ways we don’t realize.
How is nutrition related?
Our bodies operate on a delicate balance of carbohydrates, proteins, and fats, where each nutrition element is critical to our overall well-being. When there are imbalances from having either too much or too little of these nutrients, it can impact our health because our body’s priority is to protect the brain. Nutrition is also linked to stress levels and blood sugar regulation. Sometimes, we may use emotional eating or binge eating as coping mechanisms to try and address high stress.
Discovering how much our gastrointestinal system plays a part in our emotional health can be surprising. Researchers have learned that “a big part of our emotions are probably influenced by the nerves in our gut.” (3) As part of the digestive process, the microorganisms that live in our gut produce neurotransmitters like serotonin. Serotonin is closely related to mood and emotional well-being. Imbalances can contribute to depression and anxiety, which can affect our overall emotional state. It gives some validity to our “gut feelings” because “95 percent of the body’s serotonin is found in the bowels,” so it makes sense for us to become more aware of our complex relationship with food. (4)
Some strategies could help develop greater awareness of the interconnectedness of food and how our bodies function under stress: (5)
1. Think about whether you have consciously or unconsciously established rules for when you can eat or what you can eat. If you recognize some, consider when these started and why.
2. Relearn your “natural hunger cues” to help you listen to what your body says about what it needs and when it’s full.
3. Slow down and savour your food choices by noticing the flavour, textures, and feelings you experience as you eat.
- Are you enjoying the food?
- Are you responding to a craving?
- Is eating solving the problem you may have started with?
- Is your hunger going away as you eat?
- Do you feel happy, guilty, or upset while eating?
When we recognize these thought patterns, we can understand how we behave around food and be more conscious that this act to nourish ourselves is only part of a series of processes activated in our bodies.
Symptoms of stress and diabetes
Since so many are living with undiagnosed diabetes and may be unaware of the relationship between the disease and chronic stress, we thought it might be helpful to share some signs to watch for. Please keep in mind that this information is never intended to replace a diagnosis or treatment plan recommended by a health care professional.
Here are some similarities and differences between Type 1 and Type 2 diabetes:
Note: We aren’t covering other related forms of diabetes such as gestational diabetes or pre-diabetes.
We often overlook or dismiss symptoms because our lives are hectic, so and stress is so prevalent. Here are some signs of stress and what we tend to attribute them to:
Consistent and comprehensive monitoring with your healthcare team helps you identify patterns and assess how stress affects you. With this information, you can make informed plans for addressing supportive changes.
Ways to reduce stress
Reducing stress is possible by using simple but effective strategies. Embracing these adaptations to your lifestyle can make a significant difference in your long-term health and well-being.
1. Get up and move around every day.
Spend at least 150 minutes each week doing activities that increase your heart rate and get your muscles moving. You don’t have to run or do things that cause extreme exertion, and you don’t have to do marathon sessions. Tasks around the house get you moving, too. Even ten minutes of walking helps. Movement has the added advantage of improving mental health too. Before long, you may notice that your body craves it!
2. Consume a wide variety of nutritious foods that provide your body with the vitamins and minerals that chronic stress can deplete.
Getting these through food sources rather than supplementation is always preferred. You should consult a doctor or pharmacist before taking supplements to try and counteract the effects of stress or prevent diseases. Doing so could inadvertently cause more internal stress and inflammation in your body that you are unaware of and create circumstances where your body may become more vulnerable to other diseases.
3. Reduce and redirect the time spent using social media in favour of connecting with other people.
You’ll be able to practice the art of friendship, learn from other people’s perspectives, and discover what it’s like to be an active part of a community. You could participate in shared activities, interests, or experiences.
4. Explore the mechanism of your breath.
It’s easy to start by first discovering how many times you breathe in one minute and then seeing if you can reduce that by breathing fuller, deeper, and with more awareness. How do you feel when you slow your breathing down? You might prefer to use guided meditations to help your breathing and visualize what calmness is for you.
5. Seek professional help and leverage counselling to address the root causes of chronic stress you may be experiencing.
Learning about yourself and your reactions can make you better informed and anticipate and plan a better response when you encounter a stressful situation.
Discovering more about how stress and blood sugar are interconnected is a way to manage and promote good health practices and gain knowledge to live a better life.
References:
1. PAHO (Pan American Health Organization, a branch of the WHO – World Health Organization). (2022 November 11). The number of people with diabetes in the Americas has more than tripled in three decades, PAHO report says. PAHO. Retrieved December 1, 2023 from https://www.paho.org/en/news/11-11-2022-number-peo…
2. ]Cleveland Clinic (2021 December 10 – last medical review). Cortisol. Cleveland Clinic Articles. Retrieved December 1, 2023 from https://my.clevelandclinic.org/health/articles/221…
3. Mayar, E. (as cited by Hadhazy, A.) (2010 February 12). Think Twice: How the Gut’s “Second Brain” Influences Mood and Well-Being. Scientific American. Retrieved December 1, 2023 from https://www.scientificamerican.com/article/gut-sec…
4. Ibid.
5. Davidson, K. MScFN, RD, CPT (medically reviewed by Seitz, A. MS, RD.). (2020 December 3). How Can I Improve My Relationship with Food? Healthline – NUTRITION. Retrieved December 1, 2023 from https://www.healthline.com/nutrition/fixing-a-bad-…
Breaking the Silence – Navigating Men’s Mental Health Challenges and Offering Support
Breaking the Silence – Navigating Men’s Mental Health Challenges and Offering Support

There are many stereotypes of masculinity. Men are supposed to be strong and emotionally resilient, but these persistent ideals have shaped expectations placed upon men for too long. Instead, they’ve fostered a culture that tends to discourage men from expressing their vulnerability and emotions because “real men” should be stoic and unyielding. All of this directly affects men’s mental health; breaking the silence around it is a pressing imperative.
Societal and cultural influences perpetuate the myth that men seeking help for mental health struggles are weak. These ingrained beliefs have profound consequences and contribute to the alarming rates of undiagnosed and untreated mental health issues among men. It is time to recognize the need to dismantle barriers and foster an environment where men feel both empowered and encouraged to be open about their mental health. Ultimately, achieving this will pave the way for happier and healthier lives for everyone.
In this article, we’ll address the complexities of men’s mental health. We can start to break free from some of the constraints of societal and cultural influences and relieve some of the pressure that men experience that influences their reluctance and delay in seeking help for mental health. Talking about men’s mental health transparently is essential to reduce stigma. It also emphasizes the need for everyone to recognize how there is more room to be more compassionate.
How does stigma affect how men relate to mental health challenges?
Despite advances and improvements in our overall understanding of mental health, men experiencing mental health challenges often suffer alone. Stigma creates additional complexity when people struggle because they often experience “discrimination, avoidance, and rejection.” (1) It has many facets, including “social (public) stigma, self-stigma (perceived), professional stigma, and cultural stigma,” which create “extreme barrier[s]” for seeking help.(2) Many men fear being seen as less masculine or weak, which can build feelings of inadequacy and worsen their self-esteem. Stigma can influence men’s choices towards less healthy coping mechanisms like aggression or substance use to help them deal with emotional pain. Some men tend to be more comfortable focusing on physical ailments instead, which in turn delays diagnosis and treatment and creates longer recovery times.(3)
From an early age, social conditioning encourages boys to be “strong, independent and emotionally stoic, while girls are expected to be nurturing, empathetic, and compliant.”(4) The long-term effects have men “hide their vulnerabilities and suppress their emotions”.(5)
What are some notable differences in men’s mental health experiences?
The mental health challenges men experience are likely far more common than reported. For example, while depression can affect anyone, regardless of gender, there are differences in how men and women experience and exhibit symptoms. Some researchers have observed that men have more difficulty processing loss and grief over their lifetime. Many life stressors, such as physical illness, financial problems, and relationship breakdowns, become overwhelming and contribute to the manifestation of grief. (6)
Here are some differences to be aware of in how depression may present differently in men and women.
How does this information apply when people identify as Transgender, Gender Neutral/Non-Binary?
It’s critical to approach mental health with an open mind that considers gender-affirming and inclusive perspectives, recognizing that someone’s biological and psychosocial influences can vary widely and may not align with traditional expressions of symptoms of mental health challenges or distress.
- They may have coping mechanisms that depend on their unique identity and experiences and do not align with traditional gender roles.
- If they experience gender dysphoria, they feel more intense distress and depression.
- Their gender identity may influence access to mental health care and supportive services. It can affect their ability to access gender-affirming appropriate treatment. It could “create a profound sense of isolation, as they may feel misunderstood or rejected by their communities.” (9)
- They may experience chronic stress due to “fear of judgement, discrimination, or violence.” (10)
Mental health professionals need to be sensitive to the specific needs and tailor therapy that acknowledges the impact of gender identity as part of the assistance.
What do studies tell us about how prevalent mental health issues are for men?
The statistics about men’s mental health can be shocking, but being well-informed can help increase awareness of how crucial it is to change the narrative and encourage men to get the help they need.
- In the U.S., over 6 million men suffer from depression yearly. It is often underdiagnosed. (11)
- More than 3 million men in the U.S. have panic disorder, agoraphobia, or another phobia (12)
- 90% of the 3.5 million people in the U.S. who live with schizophrenia are men, diagnosed by age 30. (13)
- The highest suicide rates in the U.S. are in Caucasian men over 85. (14)
- In the U.S., gay males are at an increased risk for suicide attempts, especially before age 25. (15)
- While approximately 1 million Canadian men suffer from major depression yearly, only 30% use available mental health services. (16)
- 80% of Canadian men have spoken with a healthcare practitioner in the past 12 months as of June 2023. (17)
- Canadians were more likely to prioritize their physical health than their mental health. However, while nearly 1/3 of women selected mental health as a top priority, only ¼ of men noted the same. (18)
- 26% of Canadian men said that if they were feeling down or agitated more often than usual, they would either wait over a year or not make an appointment at all if these feelings arose. (19)
- 76% of all suicides in Canada in 2019 were by men. 38% (the highest number) were men aged 40-60. (20)
- While women attempt suicide twice as often as men, men die by suicide three times as often as women. (21)
Suicide disparities for men
Men consistently have higher suicide rates in many countries worldwide, especially in middle-aged and older age groups. They also tend to use more lethal methods that are more likely to have their attempts result in death. Targeting mental health awareness is crucial to help reduce the stigma surrounding seeking treatment for mental health challenges. At the same time, the available services must be accessible and gender sensitive. Family, workplace, and community support are essential in suicide prevention.
What are some beneficial prevention and intervention strategies?
Remember that a combination of strategies may be most effective, recognizing each person’s individual needs and circumstances.
Increasing awareness and accessibility when it comes to men’s mental health, services can work to avoid glamorizing or sensationalizing suicide through more responsible portrayals of men in the media who are dealing with mental health issues. It can also encourage more men to be open to conversations within their communities, families, and workplaces. Education can help us to:
- Recognize signs of mental health distress and promote help-seeking to destigmatize the issue.
- Ensure that access to mental health and crisis supports are available, accessible, and affordable.
- Train first responders, community leaders, teachers and medical teams to recognize men’s unique warning signs and specific risk factors such as excessive or untypical substance use or aggressive behaviour.
- Be open to developing support networks, social connections and self-help resources tailored to men’s needs and introduce the value of help-seeking and positive coping strategies to build resilience.
- Create crisis intervention plans for men who are at risk that outline what steps to take in case of a mental health emergency.
- Restrict access to weapons/firearms, medication, and other lethal means that men tend to access during crises.
Stress reduction techniques and healthy coping mechanisms can help men understand how to detect vulnerable changes in their mental health status rather than waiting for a crisis. For example, there are proven benefits of regular exercise in that it can:
- Reduce stress, anxiety, and depression.
- Improve a sense of self, boosting mood, self-worth, and self-esteem.
- Boost energy and clarity of thinking.
- Help release beneficial endorphins to clear the body of stress hormones such as cortisol.
- Be beneficial to participate in collaborative sports teams and avoid ultra-competitive/individualistic sports that build machoism.
Not discounting the value of self-care basics and engaging in enjoyable activities can also prevent crises. It may include quite apparent things but also help with releasing inhibitions that may be holding someone back:
- Getting restful sleep.
- Practicing good nutrition.
- Finding purpose through friends, family, and community involvement to forge social connections and belonging.
- Speaking with a therapist to explore supports/boundaries and develop resilience. It could also involve joining a peer support group for other men experiencing similar feelings or fulfilling similar roles and obligations.
Encouraging conversations about men’s mental health
Common stereotypes that hinder open discussions about men’s mental health include:
- The expectation that men should not show emotions, express vulnerability, or ask for help.
- The belief that men should be tough, aggressive, and dominant.
- The idea that men must be independent and self-reliant to solve all problems on their own without seeking support or help.
- The fear that admitting to mental health struggles will be seen as a weakness, failure, inadequacy, or somehow less masculine.
- The tendency to suppress strong emotions and feelings rather than address them earlier and be more proactive in looking for solutions to pain and promote recovery.
- The insensitivity of common expressions such as “man up” that trivialize normal emotional responses and promote vocabulary limitations that suppress emotional expression.
- The fear of being judged by peers, co-workers, partners, or family members if they are transparent about their mental health.
Breaking these stereotypes down helps create a supportive environment to address men’s mental health needs without fear, stigma, or judgment. We must provide safe spaces for men to discuss their feelings and share their experiences openly.
Conversation Starters
While it can be difficult for men and others, starting with an open conversation can be the best approach to take. Consider trying some of these suggestions to start a conversation if you notice someone in your life may be struggling: (22)
- How are you feeling on a scale of 1 to 10?
- You’ve been a bit quiet, how are you?
- How is work at the moment?
- When did you start feeling this way?
- How are you coping?
- Who else can you talk to?
- What help do you need?
The power of education and awareness
Some prominent men have overcome stigma and sought help, demonstrating that to do so is a sign of strength. Their stories can encourage other men to do the same.
- 1. Prince Harry has been candid about struggling with grief and mental health after his mother’s death. He co-founded the Invictus Games to promote open conversations about mental well-being and camaraderie for military service people through sport.
- 2. Comedian Trevor Noah has spoken publicly about his experiences with depression to challenge mental health stigma and promote understanding.
- 3. Actor and comedian Wayne Brady has shared his struggles with depression and anxiety to encourage other men to seek help and prioritize mental health and well-being.
- 4. Actor and former wrestler Dwayne “The Rock” Johnson has openly discussed his struggles with depression and advocates for increased mental health awareness and self-care.
We’re also sharing some resources published by the Centre for Suicide Prevention and Mental Health that you can explore. They have been specifically developed for men. (23)
Buddy Up – A men’s suicide prevention communications campaign: a call to action to men, by men
Tough Enough to Talk About It – A program for men working in trades, industry, and agriculture
Man Therapy – An interactive website that encourages men to address their mental health and seek help if necessary
DUDES Clubs – Spaces that facilitate a participant-led community for men’s wellness
HeadsUpGuys – Online information and resources to encourage help among men at risk for depression and suicide
Men’s Sheds – Community-based safe and friendly environments where men can learn practical skills, develop new interests, work on meaningful projects, connect with other men, and talk about their problems
Movember – Information about mental health and suicide prevention
Men’s mental health is not just about individual well-being. It benefits us all by creating a more inclusive, empathetic, and supportive environment. By dismantling stereotypes around men’s emotional well-being, we can help save lives, improve relationships, and promote gender equality. Supportive changes in perception will help break the silence around men’s mental health.
References:
1. Chatmon, Benita, PhD, MSN, RN, CNE. (2020 August 19). Males and Mental Health Stigma. American Journal of Men’s Health. Retrieved August 29, 2023 from ttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC7444121/
2. Ibid.
3. Duran, Andres, LPCC. (n.d.) How Mental health Stigma Impacts Men. Sage Neuroscience Centre. Retrieved August 29, 2023 from https://sageclinic.org/blog/stigma-impacts-men/
4. Hodge, Kayne. (2023, June 16). Gender Roles and Their Impact on Depression: Beyond the Surface.Mental Health Centre. Retrieved August 29, 2023 from https://www.mentalhealthcenter.org/gender-roles-an…
5. Ibid.
6. Ogrodniczuk, J. PhD. & Oliffe, J. PhD. (2011 February). Men and depression. Canadian Family Physician. Retrieved August 29, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC30388…
7. Ogrodniczuk, J. PhD. & Oliffe, J. PhD. (2011 February). Men and depression. Canadian Family Physician. Retrieved August 29, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC30388…
8. Ibid.
9. Hodge, Kayne. (2023, June 16). Gender Roles and Their Impact on Depression: Beyond the Surface.Mental Health Centre. Retrieved August 29, 2023 from https://www.mentalhealthcenter.org/gender-roles-an…
10. Ibid.
11. Mental Health America, as cited in Anxiety & Depression Association of America (ADAA) (n.d). Men’s Mental Health: Why Men’s Mental Health is Important. ADAA. Retrieved August 29, 2023 from https://adaa.org/find-help/by-demographics/mens-me…
12. Ibid.
13. Ibid.
14. Mental Health America (n.d.) Infographic: Mental Health for Men. Retrieved August 29, 2023 from https://www.mhanational.org/infographic-mental-hea…
15. Ibid.
16. Parent, A. (2023 January 26). Mental health and men: how to support your loved onesI. Canadian Red Cross Blog. Retrieved August 29, 2023 from https://www.redcross.ca/blog/2023/1/mental-health-…
17. Movember Canada as cited in CISION (2023, June 12). New Survey Suggests Positive Shift: Shows Men More Proactive in Managing their Physical Health, Continue to Struggle Prioritizing Mental Wellness. Retrieved August 29, 2023 from https://www.newswire.ca/news-releases/new-survey-s…
18. Ibid.
19. Ibid.
20. Centre for Suicide Prevention and Mental Health Commission of Canada (2022 March 30). Men and suicide. Retrieved August 29, 2023 from https://www.suicideinfo.ca/local_resource/men-and-…
21. Ibid.
22. Mental Health Innovations (n.d.) Talking about men’s mental health: conversation tips. Men’s Health Innovations Charity. Retrieved August 29, 2023 from https://giveusashout.org/latest/talking-about-mens…
23. Ibid.
Compassion Fatigue
Compassion Fatigue
You can feel that you’ve reached a limit you weren’t even aware you had. What you may be experiencing is compassion fatigue.
In this article, we’ll provide an overview of what compassion fatigue is and learn who is most often affected by it and what types of demanding professions often increase the risk/susceptibility to develop it. Compassion fatigue differs from feeling burnt out, and learning the difference between these symptoms can help create better self-awareness. We’ll also share some coping strategies and discuss how to prevent compassion fatigue. This knowledge is vital to help people experiencing compassion fatigue find strength, develop more resilience, and engage in self-care. Fundamentally, it helps us all be more compassionate towards ourselves, as well as to others.
What is compassion fatigue?
Compassion fatigue is a form of stress that someone can develop when they have direct exposure to traumatic events (firefighters, police officers, paramedics, emergency hospital staff) or secondary exposure (child protection workers, helping victimized clients, or hearing clients talking about traumatic experiences) and are focused on helping others through extraordinarily stressful or traumatic situations. The effects of compassion fatigue can result in the person being left feeling exhausted and drained, both physically and emotionally. Often, there is little room for them to take the necessary steps that would allow them to recharge and recover.
Over time, people who assist others, who “are chronically in despair” and who experience “very difficult life circumstances,” are the ones at risk of becoming “profoundly affected and even possibly damaged by their work” to the point that they may gradually experience a decline in their ability to feel empathy and compassion. (1) When that happens, there is a tendency to view the stress from these helping interactions as a routine, psychological “cost of caring.” (2)
Carers may find that they begin to “make excuses” to mask what they are feeling to justify any negative behaviours they are starting to display. Often, they will use metaphors of strength, by saying things such as – “I’ve been doing this for a very long time now, so I know how to manage it” – or – “I stayed up all night helping [this person, so] that’s why I’m a bit cranky today.” (3) The reality is that these act as “invisible badges of honour” that justify how they feel and simultaneously hide the frightening truth that they are losing control. (4) The carer’s view of the world may start to change due to repeated exposure to other people’s traumas as they begin to vicariously feel like the experiences they have been trying to help people with are now happening to them. Charles Figley, who did extensive research in these areas referred to compassion fatigue as “a dark cloud that hangs over your head wherever you go and invades your thoughts.” (5)
Compassion fatigue is treatable, especially when those directly affected, and those who care about them, begin to recognize that the root cause is that they are afraid of how their brains and bodies are telling them that they are not okay. (6)
Understanding who is most at risk
Compassion fatigue is prevalent in high-stress professions, especially roles that focus on using empathy in their pursuit of helping or serving others. It frequently affects people in the following types of occupations and roles:
- Healthcare workers (physicians, nurses)
- First responders
- Psychologists, counsellors, and social workers
- Educators
- Community service workers, foster carers
- Customer service roles
What is the difference between compassion fatigue and burnout?
While compassion fatigue and burnout are similar, there are distinct differences in where the stress originates. People who suffer from compassion fatigue have their view of the world damaged or transformed because of the work they do.
Burnout can make people more vulnerable to compassion fatigue. Burnout is when someone experiences constant mental and physical exhaustion from being in a stressful situation where they feel overworked and unappreciated. Someone with burnout may become cynical, disillusioned, and demotivated because there’s a misalignment between their job demands, responsibilities and what they value.
Unlike compassion fatigue, burnout develops from providing care and support to people experiencing trauma, resulting in diminished empathy and feeling emotionally numb.
How does compassion fatigue affect someone’s life?
Compassion fatigue can have significant repercussions in someone’s life that reach far beyond their profession. They may begin to withdraw from friends and family because they feel emotionally detached from these meaningful relationships. Compounded by their emotional exhaustion and decreased empathy, they can strain connections, leading to misunderstandings that may make them uncharacteristically seek isolation. Ultimately, they may feel challenged to separate the different aspects of their lives, and their “work habits and patterns can become increasingly unpredictable.” (7) People with strong empathy seem more at risk because they are so attuned to the vulnerabilities and suffering of those they are trying to help.
What are some of the symptoms or warning signs of compassion fatigue?
There are several warning signs that someone may be experiencing compassion fatigue. (8)
How can someone learn to cope, recognize and reduce compassion fatigue?
Someone experiencing compassion fatigue needs to recognize the toll of believing they need to stay positive and happy even when a person they are helping’s situation is challenging or worsening. In reality, it’s contradictory and unnatural to do so but there are things to do that can help them learn how to cope.
- Use self-compassion. Take the time to show yourself the same compassion you would others.
- Focus on yourself, even for a short time between interactions, to reconnect and ground yourself in your awareness and recharge. That can look like giving yourself ten minutes to complete self-care practices such as:
- Deep breathing
- Meditation
- Prayer
- Journaling
- Attend regular professional development and ongoing training, develop resiliency skills, and commit to change.
- Recognize and feel your emotions so that you can begin to release your thoughts. Allow yourself to:
- Look for and experience expressions of tension, irritability, anger
- Tell someone how you are feeling
- Prioritize giving yourself a real break. Gift yourself:
- Better work/life balance
- Vacation time
- Time for positive expressions of self-care like:
- Going for a massage
- Treating yourself to some personal care
- Watching movies or entertainment
- Spending time with friends
- And avoid potentially harmful and destructive forms such as
- Over-consuming alcohol or drugs
- Exercise has been proven to affect mental and physical health positively. When practiced regularly, it results in:
- Reductions in stress, anxiety, and depression
- Improvements in mood and self-esteem
- The natural release of beneficial endorphins that help clear cortisol, one of the body’s stress hormones
- Getting enough sleep allows your body to repair itself during the full range of a sleep cycle.
- Maintaining good nutrition with food choices and portions that are healthy, natural, and deliver sustenance, plus essential vitamins, minerals, and nutrients.
- Consider joining a support group for people who have similar roles and professional obligations that make them vulnerable to developing compassion fatigue.
- Review and rebalance workload and look for ways to increase job satisfaction, self-awareness and limit trauma inputs.
- Speak with a therapist to help you develop clear set boundaries that will help you both protect yourself and create more resilience.
- Develop a prevention plan and regularly evaluate to notice and appreciate the changes.
How can you be supportive of someone who is experiencing compassion fatigue?
Acknowledging and understanding that this phenomenon is a by-product of the carer’s role, not simply someone having a bad day, is a great way to help reduce compassion fatigue.
If you know someone who may be experiencing symptoms of compassion fatigue, you can offer help. Educate yourself so that you can recognize and provide support through:
- Develop appropriate boundary-setting
- Active listening
- Compassionate expressions of kindness and connection
- Being empathetic to them
Organizations can also reduce or prevent compassion fatigue among their staff by offering adequate education, training, compensation, benefits and access to professional help.
References:
1. Tend Academy (n.d.) What is Compassion Fatigue? tendacademy.ca. Retrieved July 23, 2023 from https://www.tendacademy.ca/what-is-compassion-fati…
2. Charles Figley 1982, as cited in Tend Academy (n.d.) What is Compassion Fatigue? tendacademy.ca. Retrieved July 23, 2023 from https://www.tendacademy.ca/what-is-compassion-fati…
3. Cunningham, Amy (2016). Drowning in Empathy: The Cost of Vicarious Trauma. TEDxSanAntonio [YouTube]. Retrieved July 23, 2023 from https://youtu.be/ZsaorjIo1Yc
4. Ibid.
5. Charles Figley, as cited in Clay, Rebecca (2022 July 11). Are you experiencing compassion fatigue? American Psychological Association. Retrieved July 23, 2023 from https://www.apa.org/topics/covid-19/compassion-fat…
6. Cunningham, Amy (2016). Drowning in Empathy: The Cost of Vicarious Trauma. TEDxSanAntonio [YouTube]. Retrieved July 23, 2023 from https://youtu.be/ZsaorjIo1Yc
7. Stowen, Debbie. (2020 November). Moving from compassion fatigue to compassion resilience. Part 4: Signs and consequences of compassion fatigue. The Canadian Veterinary Journal. Retrieved July 23, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC75607….
8. Kamkar, Katy. (2019 May 21). 20 warning signs of compassion fatigue. Canadian Occupational Safety: The Safety Magazine. Retrieved July 23, 2023 from https://www.thesafetymag.com/ca/news/opinion/20-wa…
Back to School can Bring big Changes
Back to School can Bring big Changes

Often as summer days are winding down, it’s common for children, teens, and young adults to feel anxious and develop apprehensiveness about the upcoming school year.
As parents and caregivers, it’s essential to recognize and address signs of stress and anxiety so that they can provide support and guidance. The approach they take to help is critical. They must show a clear path forward at a challenging time, while offering reassurance and tools to help them cope with their feelings. Introducing positive approaches to building confidence and creating an environment that allows their children to develop a better sense of well-being, can ease their worries and encourage them to be open-minded about the upcoming academic year.
In this article, we’ll offer some ideas about how stress and anxiety may present themselves and address possible reasons why they have cropped up. Having an approach to help work through these feelings and learn about the importance of how to care for mental health will come about through open discussion. It’s crucial to ensure your strength and resilience are healthy by modelling the need for self-care.
Recognizing signs of stress and anxiety
Sometimes, minor environmental shifts (like “back to school” signs outside retailers) can set off worry about returning to school, even if it is still weeks away. Here are some things to watch for:
- In younger children, stress and anxiety can show up as:
- Emotional outbursts.
- Insomnia or sleep troubles.
- Changes in eating habits.
- In teens and young adults, stress and anxiety might look like:
- Self-criticism and social withdrawal.
- A rejection of everyday routines and activities.
- Substance use.
What could be causing it?
- Younger children might be faced with anticipation around:
- Starting at a new school.
- Concerns around whether they will be in the same classes as their friends.
- Worrying about bullying they may have experienced or are anticipating. For example, due to changes in their health, like being unable to see or hear clearly, can build anxious feelings because they could anticipate being treated differently by peers or targeted and made fun of if they need to wear glasses or use hearing amplification devices.
For teens and young adults, there are a lot of factors to consider. Let’s look at some of the most common ones.
1. Transitioning to secondary school can be stressful.
Up to now, things have been pretty straightforward, and they may have felt confident because they were familiar with the teachers and routines.
- Secondary schools will introduce different and new approaches, expectations and accountabilities.
- Some of these may be explained in a student code of conduct that addresses items such as dress codes, attendance and disciplinary measures.
2. Competing commitments can make someone feel that they are spread too thin and creates stress. It’s essential to consider ways to support them that make the experiences “more rewarding, stimulating or pleasant,” which could initially seem counterintuitive. (1) For example, they may be comfortable combining homework and social time. To some extent, we need to trust the process and be ready to listen, offering guidance to help them navigate the many things competing for their time when they begin to show that they may be overwhelmed.
- School work
- Reinforce that learning requires dedication and focus, which comes from studying. It means that they will learn more with repeated exposure and application. Learning should be framed as continuous.
- Activities
- Participating in activities they enjoy will help them develop confidence and good self-care practices. Sports, choirs, dancing, acting, gaming, and other groups focusing on causes are just a few examples.
- Social time
- Spending time with friends has many benefits and can help them feel a sense of community and belonging.
- Work
- Consider setting limits for work hours to reinforce a priority on education and an expectation around studying and completing homework and assignments on time.
- Offer coaching to help them set appropriate boundaries with their supervisors.
- Family obligations
- Regular household operations and maintenance should be established. That might include cleaning, cooking, laundry, or cutting the lawn.
- There may be time spent as a family unit having fun on vacation, at the beach, or simply being together.
- Volunteering
- Some school boards encourage volunteerism and require several dedicated volunteer hours as a condition of graduation.
3. Nearing the end of high school can be a time when there is a lot of uncertainty and nervousness about entering a new phase of life and determining what comes next. It is important to remember that some anxiety may be caused by:
- Thinking about how they could be preparing for jobs that may not even exist yet.
- Fears:
- Of disappointing parents.
- Of being compared to siblings.
- Of finding they lack what they believe is a marker of being “successful.”
- Parents and caregivers need to consider the influence of social media in teens’ or young adults’ lives. Traditional or familiar career paths may not be part of their plans, creating conflict as it can be challenging to understand a different approach to establishing income and finding personal economic security.
- They may be struggling with anticipation around the expectations of attending post-secondary schooling, which creates tremendous amounts of stress and anxiety about:
- Needing to achieve necessary entry requirements for programs.
- Funding post-secondary education.
- Finding affordable, safe living arrangements.
- Figuring out how to suddenly be responsible for all of their own tasks that they may not be sure of yet.
4. The transition to post-secondary school.
- There are increased expectations and a more rapid approach to learning that can create pressures and take away from some of the excitement of new-found independence and accountability.
- Many students report “a decline in mental health” as the study period continues because they feel increased pressures academically, socially, and financially, which can put them at increased risk of experiencing anxiety and developing depression because of intense demands and expectations. (2)
- Parental oversight must evolve because legally and for personal and confidential reasons, they can no longer intervene with faculty and administration on behalf of their young adults.
- The onus is on students to discover and take advantage of supports and resources provided by the educational institution. Students are informed of these, and usage is highly encouraged. Sometimes, faculty may initiate a referral if they notice a student is struggling.
How to have a conversation with your child, teen, or young adult about their mental health
Parents and caregivers must be more aware of adopting positive approaches when discussing mental health to demonstrate openness and support. Children, teens, and young adults should understand that mental health is as important as physical health. Starting small and introducing the idea that regular discussion is healthy, is an excellent place to begin.
If you need help approaching the conversation around mental health, focus on keeping things simple and being supportive and open to listening to understand rather than to respond. You might even ask early in the conversation if the person wants to hear anything from you. If not, respect that may only need your time and full attention. When listening, be sure that you are non-judgemental and compassionate. (3)
- Don’t fall into the trap of stigmatizing them by making assumptions about how easy/difficult things are for young people today. It’s a sure way to disengage and shut down the conversation.
- Recognize that there may be a reluctance to be fully transparent with and bring up concerns “because they aren’t sure how parents and caregivers will react.” (4)
- Consider sharing your feelings to encourage them to open up but don’t overshare.
- You need to gauge what is age and situationally appropriate. Avoid extremes that can be overwhelming.
- Talk about mental health using people they admire or are inspired by.
- Encourage discussion even when it’s difficult or feels uncomfortable. It’s normal and healthy to do so.
- Understand that dynamics between siblings or friends significantly influence mental health.
- Always remember to see them as an individual and avoid comparisons.
- Respect their boundaries if they don’t want to share or discuss experiences or worries. Offer reassurance and reinforce trust. They need to know that they can bring things up with you when they are ready to and that your support is unconditional.
What can parents or caregivers do to be helpful, especially when this is a stressful time for everyone?
Returning to school is stressful for everyone. As parents and caregivers, it’s helpful to work through these situations, introducing healthy ways to cope and reducing some of the stress and anxiety. Be present and open to listening and learning. Above all, recognize everyone as individuals because working in generalizations and focusing on comparisons won’t be helpful.
Routines offer predictability and familiarity
Establishing or reintroducing routines a few weeks before school starts provides consistency and certainty. It is going to be beneficial to counteract uncertainty and confusion.
-
- Everyone needs to get sufficient rest to have the best chance of starting a day fresh and with optimism.
- Start with adjusting sleep schedules so bedtime and wake-up times will be closer to school schedules.
- Everyone needs to get sufficient rest to have the best chance of starting a day fresh and with optimism.
- Plan regular mealtimes to create more structure and reinforce the connection between being nourished and physical and mental health.
- Include breakfast, lunch and dinners that are healthy and nutritious.
- Book medical checkups before school starts if possible.
- Meet with a doctor to ensure your child is physically well, vaccinations are up-to-date, and you get copies of any medical records that the school may require.
- Visit an optometrist to ensure your child’s vision is optimal and, if needed, that glasses prescriptions are up-to-date.
- Schedule a dental appointment to ensure your child’s dental health is good.
- Consider preparing supplies in advance to avoid rushing and increased stress.
- For children:
- Sometimes, supply lists are available before classes start; other times, this information is shared during the early weeks of classes.
- Reduce stress by pre-planning and allowing some of your budget to go towards saving for these expenses early on.
- If funding is challenging, local resources or organizations can usually offer support.
- You can involve your child in the preparations by having them:
- Clean and organize school bags/backpacks.
- Label notebooks, pencils, pens, and lunch boxes.
- For children:
- For teens and young adults:
- Some secondary schools provide loans for digital equipment for students to use. These may be issued before orientation or during the first weeks of classes. Encourage them to call the school to find out.
- For post-secondary education, students generally provide their equipment. Still, there are usually open-access computer labs on campus and emergency loaner equipment in case of a technical malfunction.
- School network accounts may also be something students need to become familiar with to access and complete assignments.
Create a safe space for sharing feelings
Talk to your child about what they may expect for the upcoming school year. You may be surprised to hear where their focus lies. Let them lead the conversation. Work on setting a few small and easy-to-attain goals to help them realize their growth potential and how it can be achieved through their efforts. Emphasize school’s positives.
Find ways to help to reduce stress and anxiety
If there are orientations or open houses that happen in the weeks before classes start, take advantage of them. You can meet teachers and administration staff and find new or familiar faces at these events.
Introduce and model tools that can help them cope with feelings of anxiety.
This can be as simple as introducing easy-to-remember breathing and grounding techniques.
- Box breathing
- It helps some people to remember this technique if they imagine a box with four corners.
- Breathe in, counting to four slowly.
- Next, hold your breath, thinking about the air filling each of the box’s four corners.
- Then, slowly breathe out. Exhale through your nose or mouth, counting to four again.
- Finally, hold your breath for another four counts before restarting.
- Threes
- This helps calm some people by encouraging focus on their environment and where they are. The key is subtlety, quiet, and calmness.
- Look around for 3 objects. Notice them and name them quietly to yourself.
- Next, listen for 3 sounds around you. Notice them and name what they are quietly to yourself.
- Finally, notice 3 body parts that you can move. Work on gently moving each of them, slowly and carefully. It could be blinking your eyes, wiggling a finger or toes, feeling your ribs and lungs move as you breathe, or moving your head and neck slowly from side to side or in a circle.
Exercises like these reinforce resilience and are a way to remind everyone of the potential for growth, strength and what can be overcome. Practice together to reassure them and help instill confidence that they can tackle future challenges by remembering these tools.
Practice your self-care as parents and caregivers.
Ultimately, for you to be able to be intuitive, responsive, and adaptive, you need to ensure your stress levels are under control. Here are a few additional techniques and suggestions you might explore to practice better self-care.
- Make time for exercise – even ten minutes at a time. The benefits to your physical and mental health cascade and increase your capacity to find resilience and strength. Go for a short walk, get up and stretch, or dance to your favourite song.
- Get everyone involved in preparations. You don’t have to take care of everything on your own. Introduce more collaborative approaches to living and daily routines so one person doesn’t feel weighed down with responsibilities.
These approaches are beneficial because they:
- share knowledge and life skills,
- boost confidence, and
- introduces or increases independence, responsibility, and accountability.
References
1. Science Daily (2019 October 30). For teens, multitasking makes them feel better – and worse: Study finds positive emotions affect subsequent actions. Science Daily. Retrieved June 19, 2023 from https://www.sciencedaily.com/releases/2019/10/191030151514.htm
2. Moghimi, E., Stephenson, C., Gutierrez, G. et al. Mental health challenges, treatment experiences, and care needs of post-secondary students: a cross-sectional mixed-methods study. BMC Public Health 23, 655 (2023). https://doi.org/10.1186/s12889-023-15452-x
3. Brightline team (2023 March 10). 9 tips for talking to kids & teens about mental health. [Blog] Brightline. Retrieves June 19, 2023 from https://www.hellobrightline.com/blog/9-tips-for-talking-to-kids-and-teens-about-mental-health
4. Ibid.
It's not Just you. The Post-Pandemic Workplace is Stressful for Everyone
It's not Just you. The Post-Pandemic Workplace is Stressful for Everyone

Whether it takes place at home, in an office, or out on the front lines, work can be a stressful experience. In fact, Canadian workers are among the most stressed in the world.
“A lot of people don’t even realize they are experiencing moral distress. They have this general sense of outrage at the system and don’t see it for what it is.”
Work-related stress existed long before the pandemic, but it rose to new heights as our workplace fundamentals changed overnight. While the terrifying uncertainty of the early pandemic is now far behind us, the aftershocks continue to impact our mental wellbeing.
A Capterra survey found that while the percentage of Canadian employees reporting negative mental health quadrupled during the pandemic, that percentage hadn’t diminished in 2022. In fact, it had increased very slightly.
A 2022 Gallup report found that Canada is one of the most stressed regions of the world. In 2022, 44% of employees saying they experienced stress a lot of the previous day—the highest percentage in a decade.
Workers of all types are feeling stressed
Whether you perform your job remotely, on site, or on the front lines, you may be feeling work-related stress.
Nearly one in five workers in Canada are now fully remote, and while many people enjoy this work style, for others, it has created feelings of isolation and blurred the boundaries between work and life in an unhealthy way. A 2022 survey by Cisco found that stress levels had increased for more than one in five remote or hybrid workers (22%).
Many on-site workers are also struggling for reasons that include health concerns and badly-behaved customers. According to Capterra, nearly one-quarter of on-site workers (24%) rated their mental health as “bad” or “very bad.”
But first responders—the people whose work puts them in emergency situations regularly—experience some of the highest levels of work-related stress.
Alexis Winter, former Director of Nursing at Homewood Ravensview, a Canadian private mental health and addiction inpatient treatment facility on Vancouver Island, British Columbia, works with many first responders through the facility’s Guardians Program.
She agreed that the pandemic and its aftermath have worsened the mental health of front-line workers of all types.
“They’re putting their bodies on the line, and that the general population wasn’t supporting them,” Winter explained. “Health care staff were putting themselves in dangerous situations and feeling villainized. They were feeling like, ‘We don’t matter.'”
The phenomenon is directly correlated with more acute conditions such as burnout and post-traumatic stress disorder (PTSD), said Winter. Unfortunately, it’s all too easy for people to ignore the symptoms.
“A lot of people don’t even realize they are experiencing moral distress. They have this general sense of outrage at the system and don’t see it for what it is.”
The impact of work-related stress
Stress is a natural reaction to situations that seem overwhelming or threatening, priming our bodies to release stress hormones that trigger a “fight or flight” response that can protect us from danger. In a workplace setting, these situations can include physically unsafe environments, discrimination, bullying, unrealistic workloads, financial uncertainty, lack of autonomy—the list goes on and on.
But when we experience repeated exposure to these triggers over time, stress stops having a beneficial effect and starts adversely affecting our mental and physical health. In addition to anxiety, burnout, depression, and PTSD, stress can cause hair loss, memory loss, acne, hives, ulcers, heart disease, hypertension, acid reflux, headaches, insomnia, fertility issues, sexual dysfunction, obesity, and increased consumption of drugs and alcohol.
Many first responders are at elevated risk of mental health issues related to their work.
69% of Canadian journalists and media workers suffer from anxiety and 53% have sought medical help to deal with work stress and mental health.
48% of Canadian nurses say the pandemic affected their work-life balance to a great extent and 50% experienced abuse by clients or the public at work.
53% of Canadian physicians report symptoms of burnout in 2022—1.7 times higher than the pre-pandemic number.
50% of Canadian police officers reported having high levels of perceived stress.
86% of firefighters in the Northwestern Ontario fire service experienced symptoms of PTSD.
Recognizing the problem
Being able to recognize when stress is becoming harmful is critical to mental health.
People usually know when they’re stressed at work, but many see it as a normal part of having a job. If you find yourself dreading work or feeling hopeless and helpless on a regular basis, it’s a sign that your work stress may be rising to unhealthy levels.
“It’s about self-awareness,” Winter explained. “Noticing whether you’re feeling really tired, whether you’re feeling negative toward things you used to believe in. How do you feel after taking a break? Do you come back feeling good and ready to work? If you don’t feel that sense of regeneration after time away from work, it’s a sign that stress has become trauma or moral distress.”
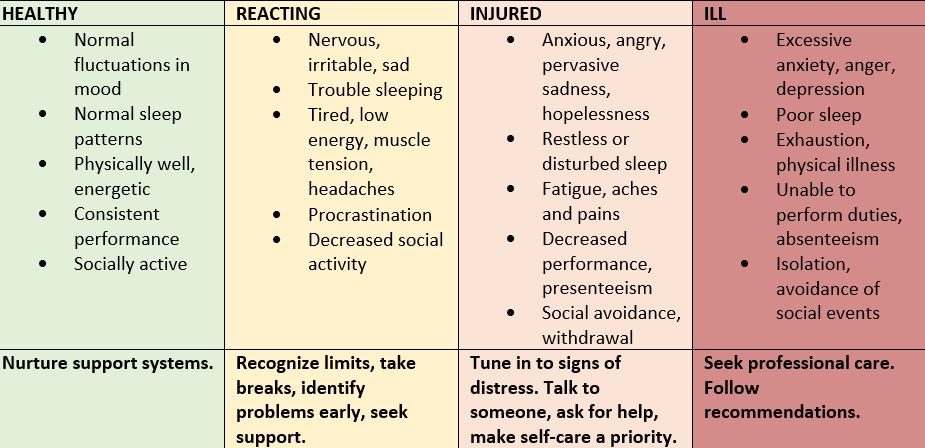
The continuum model provided by the Mental Health Commission of Canada is a helpful tool for understanding mental health as a continuum and gauging the severity of a person’s reactions to workplace stress. By evaluating yourself against each point in the continuum, you can gain a better understanding of your mental health and your potential need for lifestyle changes or professional help.
Coping with work-related stress
If your work-related stress levels are rising, there are things you can do to manage them. Here are some of the self-care strategies recommended by the team at Homewood.
Recharge. Take regular and assigned breaks at work. Take your vacation days, avoid working unnecessary overtime, and focus on rest and recovery whenever possible.
Prioritize. Know your limits. Create a routine for creating a boundary between work and the rest of your life. Make exercise, proper nutrition, and adequate sleep a priority.
Organize. Create a work environment that is tidy and organized. Break down seemingly overwhelming projects into smaller, achievable tasks.
Celebrate. Recognize and celebrate your successes (big and small) and try to keep your self-critic in check.
Connect. Seek the support of your team members or leader, and access organizational supports, such as health and counselling resources.
Winter also offers these coping mechanisms from her own practice.
Avoid relying on drugs and alcohol. “If you come home feeling really stressed out about work, don’t reach for a glass of wine or a beer immediately. Even if you only have a single glass each evening, try bringing yourself down in other ways so that using these substances doesn’t become a habit.”
Adopt a mindfulness practice. “If you’re experiencing depression, you’re living your life in the past. If you’re experiencing anxiety, you’re living your life in the future. A daily mindfulness practice, even 10 minutes before bed, helps you bring yourself into the present and alleviate those symptoms of depression and anxiety.”
Create better boundaries. “Something as simple as turning your phone off when you leave work can make a huge difference, because even that five-minute check is actually taking up 20% of your brain space for the next little while. I now have a separate work phone and a personal phone.”
Ask for help. “If you’ve taken some time away from work and you’re still feeling burned out, or if your beliefs about the safety of the world or the goodness of people has changed, it’s time to go beyond self-care and start asking for help.”
An experience we all share
Many of us are lucky enough to earn a sense of purpose from our work as well as a pay cheque. But with so much of our time and identity tied up in work activities, it’s easy for work to become a source of significant stress, and the pandemic only intensified the phenomenon. Whether we work from home, in an office, or on the front lines, it’s not uncommon for the daily grind to grind down our mental health.
What’s important is to recognize when our stress levels creep up so that we can take action, whether that involves rebalancing our work-life focus, practicing better self-care, or reaching out to people who can help us heal.
When you Fear the Unknown: Coping with Uncertainty
When you Fear the Unknown: Coping with Uncertainty

We do our best to talk ourselves into believing many different things when facing something unknown. Sometimes, we say that “everything happens for a reason,” “this too shall pass,” or “it is what it is” to calm our minds, soothe our worries, and ease our fears.
While it’s not always as simple as that, we are processing and trying to cope with uncertainty. It’s instinctive. We need reassurance and clarity to feel secure.
In this article, we’ll reframe uncertainty as a part of life that is constant and explore signs to recognize when it’s affecting us negatively. We will also investigate why we have such difficulty dealing with uncertainty, a trait referred to as Intolerance of Uncertainty (IU). There are things we can do to become more comfortable with uncertainty – since it doesn’t ever go away entirely and can resurface when you least expect it.
Uncertainty is part of life
Have you ever wondered what it would be like if our lives weren’t full of uncertainty and we had everything mapped out? It’s hard to imagine because no one comes into this world with complete blueprints for their life. Not knowing how things will play out can be a source of anxiety and can cause panic attacks.
Our brains are always on the lookout for dangerous situations. We can sense fear, and “our bodies respond automatically” to protect us. (1)
When facing uncertainty, we might experience an increased heart rate and more rapid breathing to “increase oxygen and blood going to our muscles” and sweat to control our temperature. (2) We also re-prioritize bodily functions “that aren’t immediately important” in a stressful situation and release adrenaline “to give us energy” and cortisol to both “relieve pain” and “block rational thinking” to focus on survival. (3)
Essentially, we activate our fight, flight, freeze, flop, and friend responses (4):
- Flight – responding to a dangerous situation physically or verbally
- Flight –removing yourself from the situation to put you in a safer space
- Freeze – “going tense, still and silent” as an “instinctive survival response”
- Flop – shutting down your mind in response to pain and having your muscles relax and become loose so “your body goes floppy”
- Friend – instinctively calling for help from a friend, bystander, “and/or ‘befriending’” an aggressor to try and negotiate or talk your way out of a situation
What else do we tend to do in the face of uncertainty?
Humans “crave information about the future” and “perceive ambiguity as a threat,” so our brains try to “protect us by diminishing our ability to focus on anything other than creating certainty.” (5) Think for a moment about how we have been learning to deal with uncertainties stemming from the pandemic or what we tend to do when we’re uncertain about our health and perhaps awaiting a medical diagnosis. These are stressful situations for us to figure out because they introduce changes to our regular routines.
For example, while awaiting a medical diagnosis or noticing a change in their health, many people search the Internet for information that could explain their symptoms. Unfortunately, this behaviour can result in an overwhelming amount of information, that is not always credible and can lead to more worry and uncertainty. Looking for answers is part of the quest for certainty: we can’t help ourselves.
Of course, we also can experience uncertainty in other areas of our lives. For example, “research shows that job uncertainty,” that is, worrying about our work and connected finances, is often worse than “actually losing our job.” (6)
Intolerance of Uncertainty (IU)
In some cases, extreme worry, anxiety, and stress associated with not knowing can create problems that may affect how someone handles a situation. Some people can cope with more uncertainty than others who “cannot stand even the smallest amount of uncertainty.” (7) People that are uncomfortable with uncertainty may opt to stick with familiar situations and spend much of their energy on avoiding, eliminating or controlling the negative associations they experience with uncertainty. (8) They could be viewed as perfectionists, have an “inflated sense of responsibility” or even “behave as though they have a phobia of uncertainty.” (9) In cases where anxiety creates peak amounts of distress that seriously affect someone, specialized therapy may provide some comfort and relief. The COVID-19 pandemic is a recent example of people experiencing high degrees of Intolerance of Uncertainty. Researchers have discovered that the general uncertainty associated with the pandemic correlates to excessive amounts of physiological and psychological stress, which in turn has created increased anxiety, emotional problems, depression, and other mental health concerns. (10)
Unhealthy ways of coping with uncertainty
There are several ways that people try to cope with uncertainty that are unproductive and result in more significant stress.
- Using worrying as a tool for trying to predict the future. Worrying can give you the illusion of control over uncertain circumstances.
- Compulsively seeking information can make people feel overwhelmed, depressed, or panicky. It results in a situation where it’s difficult to determine what information is credible and what is misinformation because it all creates more uncertainty.
- Isolating ourselves only results in increased feelings of anxiety and loneliness. During the early days of the pandemic, for example, when restrictions were a way to reduce the spread of infection, many people experienced anger, doubt, mistrust, and fear because they had never experienced anything similar.
How can you get more comfortable with uncertainty?
Psychologists have offered tips on how to deal with uncertainty more effectively. These include (11):
- Using self-compassion and allowing time and space to feel and experience your emotions.
- Practicing acceptance where you reflect on how life has always been uncertain.
- Staying in the present to avoid overthinking or distractions that have us examine the past or guess at the future.
- Reflecting on past experiences to address uncertainty and promote personal growth.
- Practicing self-care, embracing our instincts and self-awareness can help ground us and offer a chance to relax and recharge.
- Planning for change and uncertainty to feel better prepared to respond to future situations.
Keep things manageable by choosing three areas of focus
1. Start by focusing on what is within your control and act only on those things. If you find yourself drifting back to negative thoughts, try clearing your mind using meditation, exercising, or doing something else you love.
2. Reduce social media, news, and Internet use so you develop greater awareness of what information you are consuming and sharing. Consider that social media rarely presents authentic situations. Stick with credible sources and avoid comparisons to other people or situations.
3. Finally, focus on what brings you joy including:
- Hobbies
- Social connections
- Spending and making time for those who you determine you want in your life and where you are both benefiting from the relationship
- Gratitude journaling
- Affirmations and being kind to yourself
Being able to reframe your thinking about uncertainties in our lives may help you learn to become more content with them. You’ll reduce harmful stress and negative thought patterns and achieve better well-being, ready to embrace life with more optimism daily.
References:
1. Rape Crisis England & Wales (n.d.), The 5 Fs: fight, flight, freeze, flop and friend. Rape Crisis England & Wales. Retrieved January 20, 2023 from https://rapecrisis.org.uk/get-help/tools-for-victims-and-survivors/understanding-your-response/fight-or-flight/#:~:text=The%20%27fight%20or%20flight%27%20response,fight%27%20or%20%27flight%27.
2. Ibid.
3. Ibid.
4. Ibid.
5. Carter, Christine. (2020 July 27). Seven Ways to Cope with Uncertainty. Greater Good Magazine: Science-Based Insights For A Meaningful Life, University of California, Berkely. Retrieved January 21, 2023 from https://greatergood.berkeley.edu/article/item/seven_ways_to_cope_with_uncertainty
6. Ibid.
7. Anxiety Canada (n.d.). Intolerance of Uncertainty. Anxiety Canada. Retrieved January 21, 2023 from https://www.anxietycanada.com/articles/intolerance-of-uncertainty/
8. Psychology Tools. (n.d.) Intolerance of Uncertainty. Psychological Tools. Retrieved January 21, 2023 from https://www.psychologytools.com/resource/intolerance-of-uncertainty/
9. Ibid.
10. Russo, Francine. (2022 February 14). The Personality Trait “Intolerance of Uncertainty” Causes Anguish during COVID.” Scientific American. Retrieved on January 21, 2023 from https://www.scientificamerican.com/article/the-personality-trait-intolerance-of-uncertainty-causes-anguish-during-covid/
11.The Wellness Society. (n.d.). How to Deal with Uncertainty: 6 Tips From a Psychologist. The Wellness Society. Retrieved January 21, 2023 from https://thewellnesssociety.org/how-to-deal-with-un…
How Stigma Impacts Post-Traumatic Stress Treatment for First Responders
How Stigma Impacts Post-Traumatic Stress Treatment for First Responders

You’re the one who answers the call.
The one who shows up.
The one who offers light through life’s darkest moments.
So how could you possibly be the one feeling lost?
Feeling lost is common for First Responders, even while at work doing what they love.
If you’ve experienced feeling lost, at work or at home, you’re certainly not alone.
First Responders and Post-traumatic Stress
The Canadian Mental Health Association (CMHA) says First Responders (police, firefighters, and paramedics), military personnel, doctors, and nurses all experience higher rates of post-traumatic stress than people in other professions.
For example, twice as many First Responders compared to the average population experience a post-traumatic stress injury. That’s according to The Center for Suicide Prevention.
Dr. Jonathan Wan, MD, FRCP(C), Medical Director at Homewood Ravensview adds that this can look quite different from person to person.
General signs of post-traumatic stress, according to Dr. Wan and the CMHA, include:
- Anxiety, avoidance, and dread about attending work
- Insomnia and/or nightmares about traumatic events
- Feeling “on edge” and full of physical tension
- Apathy or having reduced interest or pleasure in spending time with others or engaging in usually enjoyable activities
- Persistent self-blame or guilt related to traumatic experiences
- Re-experiencing the traumatic event
- Feeling detached from reality or lost, disengaged, not really present
- Emotional numbness or having hard time feeling or expressing emotions
- Concentration issues (ie., brain fog)
Stigma Still Exists. You Can Fight Back.
“Unfortunately, stigma for First Responders reaching out still exists today,” says Steve Farina, City of Coquitlam Fire Captain, Vice President of Lower Mainland North at BC Professional Fire Fighters Association and Vice-Chair of the BCPFFA’s Mental Health Taskforce and Occupational Health & Safety Committee.
Stigma can be internal (ie., self-stigma) or external (ie., from peers or institutions).
Internal stigma
“The biggest barrier for reaching out seems to be self-stigma (that internal conversation where one feels weak, fearful of being judged, etc.),” says Farina.
Dr. Wan further explains that despite greater awareness related to mental health issues, reaching out can still remain difficult.
“Part of the reason is because internalized stigma can present as the negative attitudes and self-judgement we have about our own experiences,” he says.
External stigma
External stigma can come from comments said by colleagues and supervisors, or fears about what they may say or think.
Negative perceptions (ie., judgements) and harmful behaviours such as gossip towards First Responders who have experienced mental health challenges or mental health conditions are examples of external stigma, says Farina.
Dr. Wan adds that external pressures can range from peers looking unfavorably on taking time away for recovery to institutions not acknowledging the impacts of psychological injuries.
“Whatever the source, stigma can compound mental health difficulties and prevent individuals who would benefit from treatment in seeking prompt care,” he says.
Expert Advice for First Responders
Farina says his advice for any new First Responder beginning their career is to connect to a mental health professional right away.
While we understand it’s not always easy to reach out, Farina suggests there’s benefit to seeking support sooner than later.
For First Responders with post-traumatic stress injury diagnoses, the accumulation of psychological injuries in the workplace at the expense of one’s health seems to be a common occurrence, he explains.
It’s vital for First Responders to understand their health and act accordingly, adds Wan.
“The saying of putting your own oxygen mask on in a plane before helping others is a fitting analogy,” says Dr. Wan.
“Don’t wait until your backpack is full of traumatic calls and stress and you’re overwhelmed, burned out, etc.,” he says.
Farina’s suggestions:
- Find a mental health professional you can trust and relate to
- Establish a relationship and baseline history early in your career
- Check-in regularly throughout your career
Leaving symptoms of post-traumatic stress untreated can build up into a traumatic stress injury or diagnosis of PTSD.
“PTSD usually appears within three months of a traumatic event, but sometimes symptoms may not appear for years,” according to the Canadian Mental Health Association.
The benefits of working with someone at any time, according to Farina, include learning tools to:
- Destress
- Down-regulate your nervous system
- Develop the awareness to know when to take a knee and reach out for help or additional support
If you’re already experiencing early signs and symptoms of post-traumatic stress, Farina encourages you to reach out and tell your supervisor, spouse, trusted coworker, or friend.
The Homewood Ravensview Difference
Come home to yourself at Homewood Ravensview.
Since opening in 2019, we’ve helped over 400 First Responders find their path forward from post-traumatic stress injuries.
We’ve made it part of our mission to continue learning and developing programming specific to the unique needs of this critical group. We do this by learning from people who get it because they have experienced something similar and know that while every trauma experience is different, you can heal from this injury, too.
Continual Learning
In partnership with Wounded Warriors Canada, Homewood Ravensview employees were given access to specialized occupational awareness training for the treatment of trauma-exposed professionals such as members of the Canadian Armed Forces (CAF), veterans, and other First Responders (ie., police, fire, emergency service professionals, etc).
The Introduction to Trauma-Exposed Professionals training program, developed by Wounded Warriors Canada’s co-National Clinical Advisor, Dr. Tim Black, has been designed to help increase competencies in the divide that exists between trauma-exposed professionals and the public.
The training program provides culturally-specific clinical approaches to support the complex mental health needs of trauma-exposed professionals and, through our partnership, is available to all Homewood Health employees.
Healing Outside of the Uniform: Guardians Program
The Guardians program at Ravensview supports First Responders in their journey in recovery from mental health difficulties.
Highlights of Treatment
- Personalized for your unique needs
- Medication consultation and management
- Access to group and individual therapy
- Ongoing assistance from trained professionals
- Peer support from other First Responders
Treatment starts with a comprehensive and multi-disciplinary assessment to better clarify your individual needs.
You’ll gain access to individual and group talk therapy and educational tools about psychology to support your overall wellness needs.
A diverse team of physicians will then discuss ongoing interventions that can include, but are certainly not limited to, medication management.
You’ll be involved in the process of your own medical care and get the support you, too, deserve.
According to Dr. Wan, every type of treatment occurs in a therapeutic setting with other First Responders. We’ve found this promotes safety and acceptance.
Homewood Ravensview believes in the transformative power of care because we’ve seen it firsthand. If you or someone you love feels lost from trauma or PTSD, take the first step – reach out. The courage to do so could be the beginning of your path forward.
Resources
- Canadian Mental Health Association. Post-traumatic Stress Disorder.
- Steve Farina, City of Coquitlam Fire Captain, Vice President of Lower Mainland North at BC Professional Fire Fighters Association and vice-chair of the BCPFFA’s Mental Health Taskforce and Occupational Health & Safety Committee.
- Dr. Jonathan Wan, MD, FRCP(C), Medical Director at Homewood Ravensview.
- The Center for Suicide Prevention. First Responders, Trauma & Suicide.
- BC First Responders Mental Health
Reducing Holiday Stress
Reducing Holiday Stress

The holidays are a wonderful time of year. But it can also be a time when we feel the most pressured.
Here Are Some Tips to Help You Manage the Holidays:
- Manage the occasion. You may need to be more assertive and say ‘no’ to events that don’t add meaning to the holiday season for you personally.
- Clarify family expectations. This may mean not giving a gift to every grown family member or rotating who will give a gift each year.
- Lower your financial burden. Budget your spending and stick to it. If you can get through the holidays without major debt afterwards, you can enjoy the season without the guilt.
- Get organized ahead of time. Plan ahead as best as you can to get your gift wrapping and other chores done before the last minute. Then give yourself the gift of relaxation rather than stress!
- Remember that it’s the thought that counts. Don’t let competitiveness and perfectionism send you on too many shopping trips. Homemade, thoughtful, inexpensive gifts from the heart are often cherished far more than high-priced items.
- Take short relaxation breaks. If you find yourself trying to sustain a fast pace, be sure to take some down time. Just taking a few minutes to take a few deep breaths and consciously breathe away tension can be a big help.
- Make a list. Write down everything you’d like to do this holiday season and set reasonable priorities in order to get the most amount of joy from the limited amount of time you have to spend with family, friends, and co-workers. Remember, this year’s priorities may look different than those of past holidays.
- Take care of yourself. For most people, the holidays go hand-in-hand with too much sugar, fat, caffeine, and alcohol, and not nearly enough exercise and sleep. One of the best ways to combat stress is to pay attention to your body’s need for healthy food, exercise, and sleep during this busy time of year.
- Take time to laugh. If you get too stressed, take a laughter break and rent a funny holiday comedy. Laughter is the best medicine.
- Make a change. With the holiday season fast approaching, make a commitment to yourself to find a deeper satisfaction in the holiday experience. Don’t just do things because they fit into your schedule.
Instead, consider if the event or activity fits in with your values and the meaning of the season. Remember, life is really about the journey. Savour the moments — allow yourself enough time to celebrate each activity before rushing on to the next.
Don’t let the hustle and bustle of the season steal away opportunities to be thankful for the people, experiences, and events that will make this year unique and memorable. Last, but not least, commit to taking some time to reflect on the deeper meaning and spirit of the holidays for you personally, for your family, and for humanity and the world. Happy holidays!
Stress – Finding Your Balance
Stress – Finding Your Balance

Think for a moment how many times you encounter the word “stress” in a day. It could be part of your inner dialogue directly resulting from something you’re experiencing. It could be overheard in conversations around you or on TV. Let’s face it, stress (at least the kind that we’re referring to, with negative associations) is pervasive. It has such a familiar presence in our vernacular that perhaps the meaning has been diluted. Consider, though, that our body’s response to stress is instinctive. We can’t avoid it, but we can learn more about the “mechanics” of stress. With that knowledge, we can develop strategies to manage our responses.
What is stress?
Stress is a normal biological reaction to anything that requires your attention or action. Our bodies can respond to the stressor physically, emotionally, behaviourally or psychologically. It’s the response to it that can have either positive or negative effects on your health. We need stress because it helps us stay attentive and decide how best to deal with threats when they arrive. But it becomes problematic when short-term stress is prolonged.1 The conundrum is that modern life puts a lot of pressure on us. It can become difficult to remove yourself from the everyday situations that create a stressful response. The good news is that you can learn some of the common symptoms that show your body is reacting to stress. You can also learn proven techniques that will help you alleviate the pressure and offer relief.
Different types of stress
In the 1940s, Hans Selye, an Endocrinologist at McGill University, began in-depth studies of how people reacted to stressful situations and made the connection between stress and health. His theory of General Adaptation Syndrome pinpointed three main physiological stages in what would become more commonly known as the stress response:
1. Alarm – The body diverts energy to enable the “fight or flight” response. Selye observed that this initial reaction left people more vulnerable to illness because bodily systems were “offline” during this event.
2. Resistance – The body adapts to the stressor because the alarm hasn’t subsided. Energy continues to be diverted to produce stress reactions and becomes normalized.
3. Exhaustion – After prolonged stress through alarm and resistance, our immune systems become ineffective and collapse. Selye indicated that those “who experienced long-term stress could succumb to heart attacks or severe infection due to their reduced resistance to illness.”2
As these studies continued, they organized stress into four primary types: sacute, chronic, episodic acute and eustress.3
Acute
- Short term
- Positive or negative
- Encountered most frequently (day-to-day)
Episodic acute
- Acute stressors that become part of life
- Stressful episodes string together and are almost normalized
Chronic
- Always present and may seem inescapable
- For example, relationship stress or work stress
- May be caused by traumatic experiences as a child or adult
Eustress
- Positive stress that is fun and exciting
- Can keep you energized
- Provides you with surges of adrenaline
Why do you react to stress the way you do?
Have you ever wondered why some people can keep their cool during stressful situations while others fall apart or don’t notice anything at all? Differences in the stress gene can result in someone having either an overactive or underactive stress response. So, reactions can be influenced, in part, by a combination of your genetic makeup and life experiences. Learning about good or bad stress reactions can help you understand and manage stressful situations. Stress that inspires you, motivates you, or helps you enhance your performance is generally viewed as good. On the other hand, being anxious or confused, having difficulty concentrating, or having a hard time maintaining consistent performance are categorically associated with bad stress.
What about Post Traumatic Stress Disorder (PTSD)?
Traumatic life experiences can also trigger an extreme and often debilitating stress response known commonly as Post Traumatic Stress Disorder (PTSD). While we tend to think of adults as the ones who have stress invade their lives, it’s essential to consider that children are equally affected by stress. People living with PTSD may have lived experiences that cause them to react with crippling fear because of their associations with frightening or disturbing situations. Adults may find that they need to remove themselves from specific situations to avoid harmful memories and associations. Children could show sleep disturbances, fear of being alone or in certain places, or even re-enactment through play. Sometimes, we may not even be aware that a traumatic event occurred in our history. Research into trauma shows that our bodies and brains can retain the images, sounds, smells, and emotions present at the time of the event. We can be instantly transported back, resulting in a stress response. Trauma can have far-reaching effects. Studies show that childhood trauma events can manifest as chronic stress in adulthood.4
What happens in your body when you experience stress?
Stress affects your body, your mood, and your behaviour. During a stress response, the following may occur:
1. The hypothalamus at the base of your brain senses danger.
2. Your nerves send signals to your adrenal glands (on top of your kidneys).
3. Those messages quickly release a flood of chemicals and hormones such as adrenaline (also known as epinephrine)
and the primary stress hormone cortisol.
4. Your heart rate increases, sending a rush of blood to your muscles and other organs, preparing your fight/flight
(or freeze) response.
5. Your breathing increases, and you start to sweat.
6. Your body stops all insulin production to allow your muscles to be ready to use glucose fast (to flee).
The intensity and duration of stress reactions can increase your risk of developing mental and physical health problems. Frequent stress can be a contributing factor to a host of health conditions, including, but not limited to:
- Diabetes – insulin resistance
- Hypertension – damaged blood vessels
- Heart attack or stroke – stress increases the risk of occurrence
Stress has also been linked to:
- Headaches
- Substance use problems
- Anxiety, depression
- Insomnia
- Weight gain
- Changes in mood, energy, and libido
- Hair loss
- Muscle tension, especially in the neck and shoulders
- Grinding teeth, gum disease
- Ulcers and digestive system issues such as diverticulosis/diverticulitis
What are some of the best things to do to reduce stress quickly?
Remember that our stress response floods our bodies with chemicals and hormones. We need to flush them from our systems to counteract the effects of the fight/flight/freeze response to regain control. There are three actions that may provide almost immediate relief.
- The first is to move. Exercise releases endorphins into your bloodstream even after only one minute of activity.
- The second is to become aware of the connection between your mind, body and breathing. Meditation and other mindfulness practices such as yoga and tai chi teach you to introduce calm voluntarily by becoming more aware of your senses and body movements.
- The third is to listen to calm music to lower blood pressure and reduce cortisol.
What are some ways to manage long-term stress?
You can take a proactive approach to manage stress by setting boundaries in your work, personal life, and community. These tend to be sources of acute or chronic stress. Taking stock of how you feel, then adjusting your behaviours can eliminate or alleviate self-imposed pressure. One clinical psychologist observed that “we don’t help anyone by getting burnt out and needing care ourselves. It is what makes these boundaries so important. We have to decide how much we can give to our friends, family and communities before we stop to recharge our own batteries with time away.”5
- Consider planning your tasks and finishing your workday
at a specific time. You can also commit to eating well and exercising by scheduling time for them in your calendar and tracking how frequently you complete them. - On the personal front, be aware of friends that drain you. When you find that you are always the one who is listening, let them express themselves but tell them that they need to reciprocate. You may also feel better by reducing the amount of time you spend viewing screens and aimlessly scrolling through social media posts. Instead, get in touch with your creative side. You’ll feel more productive and reward yourself with personal growth.
- Many times, we’re stretched too thin. Allow yourself to skip community events guilt-free. Take up a new hobby or permit yourself to do something you love in the time that you would have spent doing something else. You don’t need a full social calendar. If something makes you feel uneasy, listen to your instincts. It’s okay to disconnect or change the format.
What about the often-elusive notion of balance? Is it achievable?
We’re told that it’s crucial to find a balance between our work and personal lives, two competing priorities. There are times when one will demand more time and attention than the other. It may not be entirely realistic to imagine that you can devote equal attention to both. Instead, consider that finding balance may not be the ideal approach. Focusing on finding harmony so that everything in your life can co-exist can be a less stressful approach. The notion of harmony “invokes the idea that you should enjoy work and life at the rhythm that makes the most sense for you and what’s taking place in your life at any given time.”6 A happy product of shifting the focus from balance to harmony is a revival of creative thinking, problem-solving, and planning, reducing procrastination and learning to be better at asking for help.
Harmony also gives you room to find your passion. For example, you can envision your dream job, but also consider doing something that you always wanted to try but talked yourself out of doing. You can also revisit some of your favourite things. Think about what you enjoyed when you were young. Consider trying something related but different from something you already know how to do. These visioning exercises allow you to flex your brain to find some inspiration.
Good wellness practices and habits can help
When you strive to incorporate better wellness in your life, you become more self-aware and better able to control responses and reactions. It’s developing a habit of being kind to yourself, otherwise known as self-care. Start by reviewing how much you are taking on. Could you do things differently? Perhaps more leisurely? Consider whether you need to be the one doing a particular task. You can start by building good habits systematically to help you reduce stress, such as:
- Get good sleep. Good sleep hygiene includes having a calm space and a dark, cool room. Set yourself a respective bed time and remove electronics to reduce blue-light emissions and radio frequencies that can affect your brain and your ability to get to and stay asleep.
- Nutrition. Avoid caffeine, especially before bedtime. Instead, try drinking green tea, which releases theanine to calm your nervous system.
- Exercise. Working out doesn’t need to be done in a big session at all. Just move! Even 10 minutes at a time can add up over a day. If you can’t find 10 minutes, go for a two-minute walk.
- Try some
balanced breathing techniques to relax. Start by inhaling through your nose for a count of four, then holding that breath for another four-count. Then release that breath through your mouth for a count of eight. Repeat the process several times for the greatest benefit. It is an excellent way to reduce your heart rate and blood pressure. - Find something to
laugh about. It helps reduce stress by bringing air into your body and reducing tension in your circulatory system and muscles. - Singing has been proven to reduce cortisol and help you feel more relaxed. It can also boost your mood, increase your brain activity, and control your breathing.
- Finally, don’t underestimate the power of a good conversation. Talking to friends about what’s causing you stress can be helpful as you can hear different perspectives and recommendations that you may not have considered. There’s also merit in “talking” to yourself through journaling. Over time, you can reflect on earlier journal entries.
References:
1. Scott, Elizabeth, PhD. (2020 August 3). What Is Stress? Part of How Stress Impacts Your Health Guide. verywellmind. Retrieved on January 12, 2022 from
https://www.verywellmind.com/stress-and-health-314…
2. Centre for Studies on Human Stress (CSHS). (n.d.). History of Stress: Close-up on…The General Adaptation Syndrome. Retrieved on January 12, 2022 from
https://humanstress.ca/stress/what-is-stress/histo…
3. Scott, Elizabeth, PhD. (2020 August 3). What Is Stress? Part of How Stress Impacts Your Health Guide. verywellmind. Retrieved on January 12, 2022 from
https://www.verywellmind.com/stress-and-health-314…
4. van der Kolk, B. M.D. (n.d.) The Body Keeps The Score: Brain, Mind, and Body In The Healing Of Trauma. Retrieved on January 14, 2022 from
https://www.besselvanderkolk.com/resources/the-bod…
5. Ali, S. (2021, March 12). Establishing These 4 Types of Boundaries Can Help Alleviate Stress, Says a Psychologist. Self-care Tips from Well + Good. Retrieved on January 14, 2022 from
https://www.wellandgood.com/stress-boundaries/
6. Vetter, A. (2017, October 24). If Work-Life Balance Isn’t Realistic, Try This Instead. Entrepreneur. Retrieved on January 14, 2022 from
https://www.entrepreneur.com/article/300060
Mental Health Checkup: Preparing for the year ahead
Mental Health Checkup: Preparing for the year ahead

A new year is nearly upon us. Traditionally, this is a time when many of us reflect on the previous year and make “resolutions,” or plans for the coming year. The stresses associated with the pandemic, including job losses; economic uncertainty; deaths of family members, friends or colleagues; burnout; restricted social interactions and the instability, uncertainty and fear have impacted the mental health of many. (1)
With vaccination efforts and continued vigilance, we have largely brought case numbers under control. With the pandemic having shaped our lives for the past two years, psychologists are concerned about the long-term impacts of COVID-19 on mental health, and rightly so. Past traumatic events such as natural disasters, the global economic downturn and other public health crises, such as SARS, led to lasting detrimental impacts on mental health (2) and were associated with increased rates of substance abuse, PTSD and depression. (3)
Burnout and reflection on the past year
Think about your daily routines of the past two years. You may have started your day scrolling social media and news apps, followed by working from home (video calls, sitting in front of a screen or two), helping children with online school, troubleshooting tech issues, texting, DMs, Skype or Facetime with family and ending the day with more “doomscrolling” before falling into a fitful sleep. And those days all seemed to blur together—how many times have you said “What day is it today?”
While burnout, a state of emotional, physical and mental health exhaustion caused by excessive and prolonged stress, (4) has always been around, it’s increased during the pandemic. Our work-life balance was suddenly tipped when we started “living at work” with our kitchen tables acting as our makeshift offices.
In a recent survey, 85% of respondents said their well-being had declined, 62% were struggling to meet their workload and balance work with other responsibilities, and exhaustion and cynicism were on the rise. (5)
While digital devices were a lifesaver during the pandemic—time spent on digital devices increased from 17% on gaming consoles to 45% on laptops and 76% on smartphones—they contributed to digital fatigue or digital burnout: the state of mental exhaustion from using multiple digital tools leading to lack of energy, mind fragmentation and burnout. (6)
In addition to living through a pandemic for the past two years, and all the challenges that came with it, we’ve been inundated with negative news. As events unfolded in the United States after the high-profile killings of Ahmaud Arbery, Breonna Taylor, George Floyd and others, (7) protests and political tensions escalated, including the insurrection at the US Capitol building in January 2021. In the spring, many non-Indigenous Canadians were shocked by the discovery of unmarked and mass graves of children at former Residential School sites, with Indigenous communities retraumatized by the news.
Climate change—largely forgotten during the pandemic—became front and center again in early summer as record-breaking heat in Western Canada was followed by wildfires that ravaged towns and communities leaving many without homes or jobs. (8)
Even though some of us may not be aware of it, these events, digital burnout, struggles with work-life balance, as well as the pandemic itself, have impacted our mental health and may have caused us to abandon our healthy coping strategies.
With that in mind, and as we start to come out the other side of the pandemic, the new year is an excellent time to check-in and prioritize your mental health and make realistic goals for the coming year.
What does “checking in” with your mental health mean?
First of all, what does mental health mean? As the World Health Organization defines it, “mental health is a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to society”. (9) It doesn’t mean that you’re happy all the time—good mental health means experiencing a full range of emotions. Our mental health affects how we think, feel, act, relate to others and our decision-making. It includes our emotional, psychological and social well-being. Poor mental health affects our physical health too; depression increases the risk for stroke, type 2 diabetes and heart disease. (10)
It’s important to recognize that there’s a difference between mental health and mental illness. Mental illness refers to a number of medical conditions; much like heart disease or diabetes are medical conditions. Mental illnesses involve changes in emotion, thinking and behaviour and are associated with distress and or problems functioning in social, work or family activities. They include depression, anxiety disorders, eating disorders and addictive behaviors. (11)
Mental health problems, when left unchecked, can become a mental illness
Checking in with your mental health is a way to determine and acknowledge how you’re actually doing. To start your mental health check-in, take some time to reflect on the following. If you notice a shift away from what is typical for you, it’s a warning to make changes to improve your mental health.
- How are your sleep patterns? Are you sleeping more often than usual or less?
- What is your appetite like? Are you eating more or less causing changes in weight?
- How is your energy level? Is it high or low? Do you find yourself watching another show on Netflix rather than getting up and exercising, going for a walk or even cleaning the house?
- Are you able to concentrate, or do you find yourself distracted?
- Are you feeling optimistic about the coming year? Or pessimistic?
- Are you participating in and enjoying activities and people? Many of your usual activities may not be available, but there are alternatives. Are you making efforts to shift to things you can do, such as walking, hiking, biking, virtual book club meetings, small outdoor gatherings, outdoor dining, etc.?
- Is your mood low or high? Are you having difficulty getting out of bed because of your mood?
- Are you irritable or feeling angry? Do you find yourself getting into arguments or yelling?
While we may all have an “off day,” if you find that you’re experiencing negative changes in your daily life for two weeks or more, it may be time to seek help.
Strategies to prepare for the year ahead
Reflecting on the emotions and experiences you’ve had during the past two years can help you build awareness and develop skills to improve your mental health. Identify the highest stress triggers, especially those during the pandemic. Some of these may have been resolved already; your children may be back at school and the pandemic news isn’t as gloomy every day. Look at the results of your mental health check in and consider how you can make improvements. Look at the start of the new year as a clean slate and a new beginning with new goals.
Build on what you found most important during the pandemic or what you missed the most. One upside to the pandemic is that for some people, the pandemic created space to slow down, spend time with family, refocus on what’s important, and connect with one another in new ways. Itai Danovitch, MD, chair of the Department of Psychiatry and Behavioral Neurosciences at Cedars-Sinai points out that events like the pandemic can lead to growth. “People develop resilience. They learn how to deal with mental health challenges, and they find resources, internal and external, that they didn’t know existed.” (12)
The following can help you create an achievable action plan for the coming year that can help improve your mental health:
Digital hygiene
- Delete apps from your phone. Do you need to have all those news and social media apps at your fingertips? If these have been a source of distraction and doomscrolling, delete them! You can reinstall them later when you feel back on track. If you want to keep your apps, set time limits and ensure that you stick to them.
- If you’re working from home and feel you haven’t created a good work-life balance, set boundaries between your personal life and work life. When your workday is done, power off your laptop, close it up and put it and your files away. You’ll be less tempted to “just check your email” if you have to power on your computer.
- Take frequent breaks from screen use and structure time in your workday for offline work.
Set realistic, achievable and specific goals
- Creating goals is an excellent way to improve your sleep, eating habits, and exercise and activity regime. If your goals are too vague (such as, “get better sleep” or “eat better”), it’s difficult to achieve them. What defines better sleep for you? A more specific and achievable goal would be: “Lights out by 10 and leave my phone/laptop/tablet downstairs at night.”
- Write down your goals to hold yourself accountable and keep track of your progress.
Get active
- One of the most effective ways to improve your mental health is regular activity and exercise. Again, set realistic, achievable and specific goals to jump start your activity.
- Recruit family members to join you or plan regular socially distanced activities with friends. Walking, biking, jogging/running, skiing and yoga are activities that you can gradually increase the intensity of as your fitness level increases.
- Set reminders in your phone to take short breaks to stretch or walk around your home/office throughout your workday.
- Have a back-up plan for activities you can do inside during inclement weather (reading, baking, cooking, and even cleaning).
Improve your concentration
- Use to-do lists and prioritize your top tasks for each day. Adjust your list as the week goes on and your priorities change.
- Focus on one task at a time; avoid jumping from task to task or multi-tasking.
- Set scheduled breaks to stretch or go for a short walk to clear your mind.
- Organize your desk to remove distracting clutter. Put your phone away so you’re not tempted to check messages.
Make plans for the coming year
- As venues and travel begin to open up, make plans. Even if you’re hesitant about international travel or large indoor events, you can choose smaller events and gatherings with small group of friends. It’s okay to feel hesitant about going to a party at a friend’s house or attending a concert or play, even if others in your circle are taking the leap. Take small steps by grabbing a quick coffee with friends or having a friend over for a movie.
- Make travel plans closer to home; there are likely lots of unexplored places close to home and you can take advantage of this time to check out places you’ve heard of, but never visited.
- Prioritize safe visits with people important to you; whether that’s family or friends.
You may find that as parts of your life slowly return to normal, you begin to feel the impacts of everything we’ve collectively experienced. You need to determine what you need to recover and heal from what’s been a very difficult time. Everyone’s different and what works for your family or friends, may not work for you. That’s okay. Self-compassion and self-care are essential, as well as time to adjust to post-pandemic life.
If you find that you or someone you care about is consistently in a low mood, lashing out or doesn’t know how to start making changes, speak to your primary care giver, or contact your Employee Family Assistance Program for options available to you. You are not alone.
References:
- Abbott, A. (2021, February 3) COVID’s mental-health toll: how scientists are tracking a surge in depression. Retrieved on June 22, 2021 from
https://www.nature.com/articles/d41586-021-00175-z - Savage, M. (2020, October 28) Coronavirus: the possible long-term mental health impacts. Retrieved on June 23, 2021 from https://www.bbc.com/worklife/article/20201021-coronavirus-the-possible-long-term-mental-health-impacts
- Cedars Sinai. (2020, November 24) Long-term impacts of COVID-19: your mental health. Retrieved on July 7, 2021 from https://www.cedars-sinai.org/newsroom/long-term-impacts-of-covid-19-your-mental-health/
- Queen, D. and K. Harding. (2020, July 6) Societal pandemic burnout: a COVID legacy. Retrieved on June 23, 2021 from https://onlinelibrary.wiley.com/doi/full/10.1111/iwj.13441
- Beheshti, N. (2021, March 11) Is pandemic burnout draining your motivation and energy? Here’s how we can all promote recovery. Retrieved on June 23, 2021 from https://www.forbes.com/sites/nazbeheshti/2021/03/11/is-pandemic-burnout-draining-your-motivation-and-energy-heres-how-we-can-all-promote-recovery/?sh=5b3e41b91c02
- Sharma, M.K., et al. Digital burnout: COVID-19 lockdown mediates excessive technology use stress. WorldSoc Psychiatry. 2020: 2:171-2. Retrieved on June 24, 2021 from https://www.researchgate.net/publication/343724873_Digital_Burnout_COVID-19_Lockdown_Mediates_Excessive_Technology_Use_Stress
- Dungca, N., J. Abelson, M. Berman, J. Sullivan. (2020, June 8) A dozen high-profile fatal encounters that have galvanized protests nationwide. Retrieved on July 6, 2021 from https://www.washingtonpost.com/investigations/a-dozen-high-profile-fatal-encounters-that-have-galvanized-protests-nationwide/2020/06/08/4fdbfc9c-a72f-11ea-b473-04905b1af82b_story.html
- Baum, K.B., I. Semeniuk, M. McClearn. (2021, July 1) B.C.s heat wave and fires were driven by climate change, and they won’t be the last. What must we do next? Globe and Mail. Retrieved on July 7, 2021 from https://www.theglobeandmail.com/canada/article-western-canadas-deadly-heat-wave-is-driven-by-climate-change-will-it/
- WHO. (2018, March 30) Mental health: strengthening our response. Retrieved on June 22, 2021 from https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
- CDC. (n.d.) Learn about mental health. Retrieved on June 22, 2021 from https://www.cdc.gov/mentalhealth/learn/index.htm
- Mayo Clinic. Mental illness. Retrieved on July 6, 2021 from https://www.mayoclinic.org/diseases-conditions/mental-illness/symptoms-causes/syc-20374968
- Cedars-Sinai. (2020, November 24) Long-term impacts of COVID-19: your mental health. Retrieved on July 7, 2021 from https://www.cedars-sinai.org/newsroom/long-term-impacts-of-covid-19-your-mental-health/




