Moral Injury in Healthcare and the Role of Self-care
The traumatic legacy of the pandemic continues to impact the mental health of Canadian healthcare workers who put their lives on the line. Practicing self-care can help them heal.
July 24 is Self-Care Day, a day to recognize the importance of self-care in empowering people to look after their own health. For healthcare professionals in Canada, it’s a day to explore the ways in which self-care can play a role in helping to manage the toll that this important work can take on their mental health.
Dr. Tara Riddell is a psychiatrist for the Addiction Medicine Program and the physician wellness lead at the Homewood Health Centre, a leading inpatient treatment facility in Guelph, Ontario, that focuses on mental health, trauma, and addiction. She began exploring the relationship between mental health and self-care early in her career.
“In medical school, I started my research with the goal of reducing stigma related to mental health amongst the general population,” she explained. “But I soon recognized that this was a significant issue for myself and my healthcare colleagues, who have high rates of burnout, depression, anxiety, and suicide risk. I began to think about how I could take care of myself throughout my career journey and what other healthcare professionals may need to feel well and fulfilled in the work that we’re doing.”
Stress management for healthcare professionals has always been a challenge, but when the pandemic struck, the situation rose to crisis levels.
 Moral injury: The pandemic legacy
Moral injury: The pandemic legacy
In 2020, psychological distress in healthcare began to make headlines. As healthcare professionals all over the world risked their lives to continue delivering care under trying circumstances, their mental health suffered, and the rates of moral injury soared.
Moral injury is a type of stress caused when a situation forces a person to behave in ways that go against their moral code. Its impact on mental health is profound, and it can result in depression, anxiety, and post-traumatic stress disorder (PTSD) for healthcare professionals.
According to data collected in 2022, Canadian healthcare providers were exposed to a host of morally injurious events during the pandemic, including watching their patients die alone, witnessing patient harm, being exposed to bullying and violence, not having access to adequate resources and personal protective equipment, and coping with increased workloads and decreased staffing. In one study, a staggering 81% of Canadian healthcare workers said they were exposed to an unethical culture, 55% said they were exposed to a low psychosocial safety climate, and 50% said the quality of care was hindered.
As a result, the rates of moral injury for healthcare professionals in Canada rose dramatically. An online survey of Canadian physicians conducted in 2020 found one-third of respondents had considered leaving or previously left a position because of moral distress and another one-third met the criteria for burnout syndrome. In another survey of Canadian healthcare workers conducted in 2022, 25% had considered leaving their profession due to moral distress, 25% met the criteria for PTSD, and 60% had significant levels of depression.
A resistance to self-care
Dr. Riddell is quick to stress that solving the issue of moral injury in Canadian healthcare requires systemic change, including more resources, a bigger workforce, and improving the coordination of care. But she is also a strong proponent of practicing personal self-care as a way to manage stress and prevent burnout and moral injury.
However, healthcare professionals have a tendency to resist this approach. “Healthcare is not a culture that has been compassionate to our own vulnerability or suffering or perceived weakness, or even the disclosure at work of mental health challenges or concerns,” she said. “Sometimes it can be very challenging for health care providers to engage in self care, because we feel guilty for it, or we feel it is selfish. But in order to be at your full capacity to help others, you need to take care of your own needs first.”
From shame to acceptance
Removing the stigma around mental health is a crucial part of the process. Ironically, healthcare workers who treat their own patients with tremendous understanding often feel shame around their own mental health issues.
But extending the same sense of compassion to ourselves that we extend to our patients is the foundation for effective self care. Dr. Riddell said that when we see the difficulties or challenges we experience as part of a shared human experience, it can reduce the stigma and break down barriers.
“It allows me to have more open conversations with colleagues about something that’s weighing on me and to recognize that I’m not any ‘less-than’ as a health care provider for having some of these challenges. It helps me shed some of the shame and do a little bit of internal healing.”
Healthcare Salute, a resource for healthcare professionals who may be experiencing or at risk of moral injury, provides a helpful mental health model to help people self-assess their mental health and determine the actions they can take to improve it. The model is also intended to reduce the stigma around mental health issues by placing the full range of experiences on a continuum.
The Mental Health Continuum
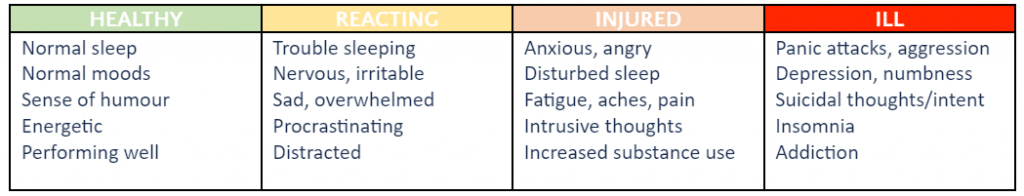
(This table is condensed and adapted from the Mental Health Continuum Model developed by Healthcare Salute. See the full continuum here.)
 Five ways to practice self-care
Five ways to practice self-care
Dr. Riddell believes that every healthcare professional can benefit from practicing self-care, no matter where they fall on the continuum of mental health.
“I often use the image of an internal tank,” she explained. “Through personal and especially professional responsibilities, our tank has lots of little drains. When our tank becomes depleted, we begin to experience greater challenges, and that’s where we may experience burnout or other mental health concerns. Self-care is a way to help refill our tank, or at the very least slow some of those drains.”
Dr. Riddell recommends these simple self-care tactics as a way for healthcare professionals to make small changes that can protect their mental health and replenish their internal tank.
Take ten. “I think everyone in healthcare has skipped a meal or a snack break or a bathroom break. Sometimes self-care means saying, ‘I may be late, but I need to take care of a basic need. If I take ten minutes to have a snack or lunch, I’m going to feel better and I’ll be able to be more present with the person I’m meeting with next.”
Try mindfulness. “In Homewood Health Centre’s Addiction Medicine Program, many of our healthcare providers incorporate mindfulness into their day. In times of heightened distress, they utilize deep breathing, attend to their own emotions, and practice ways of grounding themselves.”
Go offline. “My colleagues are increasingly finding ways to set limits on the work we do. I’m seeing staff identify when they’re going to be offline and indicate that they won’t be responding until a later date so that they have that protected time to recover.”
Reach out. “Social connection and engagement, especially with people who are also going through similar experiences, is an important way to foster self care. Social well being is one of the components of our wellness.”
Set priorities. “Increasingly, for all of us, time is a very scarce commodity. I try to think about how I’m using my time, and whether the things that are taking up my time are ultimately aligned with my core values. If they are, I’m more likely to feel a sense of enjoyment from doing it or a sense of fulfillment and meaning. And that helps me refill my tank.”
From “work warrior” to “wellness warrior”
People choose careers in healthcare because they want to nurture the health of others, but the soaring rates of moral injury for Canadian healthcare providers has shown that we’re not always as attentive to our own health. While self-care can’t mend a healthcare system in crisis, it can help those who work within it to protect their precious mental health.
“In our culture, we’ve often celebrated the work warrior, the person who is always taking on new challenges, never stops, and sacrifices their own needs,” Dr. Riddell pointed out. “Maybe we should be celebrating people who are prioritizing their wellness because they know that’s what they need and is going to be beneficial to their team and to patients.”
More self-care insights and ideas
An ongoing Canadian national study is now investigating the causes and impact of moral injury in Canadian healthcare professionals. The study involves a collaboration between Homewood Health, which has donated funds and expertise, the Homewood Research Institute, McMaster University’s Department of Health Sciences – Psychiatry and Behavioural Neurosciences, Atlas Institute for Veterans and Families, St. Joseph’s Healthcare, Western University, IDEaS, and the Public Health Agency of Canada.
As part of the project, Healthcare Salute was launched to share information, resources, and stories to help HCPs get the support they need to connect, self-assess, and practice self-care.
