When you Fear the Unknown: Coping with Uncertainty
When you Fear the Unknown: Coping with Uncertainty

We do our best to talk ourselves into believing many different things when facing something unknown. Sometimes, we say that “everything happens for a reason,” “this too shall pass,” or “it is what it is” to calm our minds, soothe our worries, and ease our fears.
While it’s not always as simple as that, we are processing and trying to cope with uncertainty. It’s instinctive. We need reassurance and clarity to feel secure.
In this article, we’ll reframe uncertainty as a part of life that is constant and explore signs to recognize when it’s affecting us negatively. We will also investigate why we have such difficulty dealing with uncertainty, a trait referred to as Intolerance of Uncertainty (IU). There are things we can do to become more comfortable with uncertainty – since it doesn’t ever go away entirely and can resurface when you least expect it.
Uncertainty is part of life
Have you ever wondered what it would be like if our lives weren’t full of uncertainty and we had everything mapped out? It’s hard to imagine because no one comes into this world with complete blueprints for their life. Not knowing how things will play out can be a source of anxiety and can cause panic attacks.
Our brains are always on the lookout for dangerous situations. We can sense fear, and “our bodies respond automatically” to protect us. (1)
When facing uncertainty, we might experience an increased heart rate and more rapid breathing to “increase oxygen and blood going to our muscles” and sweat to control our temperature. (2) We also re-prioritize bodily functions “that aren’t immediately important” in a stressful situation and release adrenaline “to give us energy” and cortisol to both “relieve pain” and “block rational thinking” to focus on survival. (3)
Essentially, we activate our fight, flight, freeze, flop, and friend responses (4):
- Flight – responding to a dangerous situation physically or verbally
- Flight –removing yourself from the situation to put you in a safer space
- Freeze – “going tense, still and silent” as an “instinctive survival response”
- Flop – shutting down your mind in response to pain and having your muscles relax and become loose so “your body goes floppy”
- Friend – instinctively calling for help from a friend, bystander, “and/or ‘befriending’” an aggressor to try and negotiate or talk your way out of a situation
What else do we tend to do in the face of uncertainty?
Humans “crave information about the future” and “perceive ambiguity as a threat,” so our brains try to “protect us by diminishing our ability to focus on anything other than creating certainty.” (5) Think for a moment about how we have been learning to deal with uncertainties stemming from the pandemic or what we tend to do when we’re uncertain about our health and perhaps awaiting a medical diagnosis. These are stressful situations for us to figure out because they introduce changes to our regular routines.
For example, while awaiting a medical diagnosis or noticing a change in their health, many people search the Internet for information that could explain their symptoms. Unfortunately, this behaviour can result in an overwhelming amount of information, that is not always credible and can lead to more worry and uncertainty. Looking for answers is part of the quest for certainty: we can’t help ourselves.
Of course, we also can experience uncertainty in other areas of our lives. For example, “research shows that job uncertainty,” that is, worrying about our work and connected finances, is often worse than “actually losing our job.” (6)
Intolerance of Uncertainty (IU)
In some cases, extreme worry, anxiety, and stress associated with not knowing can create problems that may affect how someone handles a situation. Some people can cope with more uncertainty than others who “cannot stand even the smallest amount of uncertainty.” (7) People that are uncomfortable with uncertainty may opt to stick with familiar situations and spend much of their energy on avoiding, eliminating or controlling the negative associations they experience with uncertainty. (8) They could be viewed as perfectionists, have an “inflated sense of responsibility” or even “behave as though they have a phobia of uncertainty.” (9) In cases where anxiety creates peak amounts of distress that seriously affect someone, specialized therapy may provide some comfort and relief. The COVID-19 pandemic is a recent example of people experiencing high degrees of Intolerance of Uncertainty. Researchers have discovered that the general uncertainty associated with the pandemic correlates to excessive amounts of physiological and psychological stress, which in turn has created increased anxiety, emotional problems, depression, and other mental health concerns. (10)
Unhealthy ways of coping with uncertainty
There are several ways that people try to cope with uncertainty that are unproductive and result in more significant stress.
- Using worrying as a tool for trying to predict the future. Worrying can give you the illusion of control over uncertain circumstances.
- Compulsively seeking information can make people feel overwhelmed, depressed, or panicky. It results in a situation where it’s difficult to determine what information is credible and what is misinformation because it all creates more uncertainty.
- Isolating ourselves only results in increased feelings of anxiety and loneliness. During the early days of the pandemic, for example, when restrictions were a way to reduce the spread of infection, many people experienced anger, doubt, mistrust, and fear because they had never experienced anything similar.
How can you get more comfortable with uncertainty?
Psychologists have offered tips on how to deal with uncertainty more effectively. These include (11):
- Using self-compassion and allowing time and space to feel and experience your emotions.
- Practicing acceptance where you reflect on how life has always been uncertain.
- Staying in the present to avoid overthinking or distractions that have us examine the past or guess at the future.
- Reflecting on past experiences to address uncertainty and promote personal growth.
- Practicing self-care, embracing our instincts and self-awareness can help ground us and offer a chance to relax and recharge.
- Planning for change and uncertainty to feel better prepared to respond to future situations.
Keep things manageable by choosing three areas of focus
1. Start by focusing on what is within your control and act only on those things. If you find yourself drifting back to negative thoughts, try clearing your mind using meditation, exercising, or doing something else you love.
2. Reduce social media, news, and Internet use so you develop greater awareness of what information you are consuming and sharing. Consider that social media rarely presents authentic situations. Stick with credible sources and avoid comparisons to other people or situations.
3. Finally, focus on what brings you joy including:
- Hobbies
- Social connections
- Spending and making time for those who you determine you want in your life and where you are both benefiting from the relationship
- Gratitude journaling
- Affirmations and being kind to yourself
Being able to reframe your thinking about uncertainties in our lives may help you learn to become more content with them. You’ll reduce harmful stress and negative thought patterns and achieve better well-being, ready to embrace life with more optimism daily.
References:
1. Rape Crisis England & Wales (n.d.), The 5 Fs: fight, flight, freeze, flop and friend. Rape Crisis England & Wales. Retrieved January 20, 2023 from https://rapecrisis.org.uk/get-help/tools-for-victims-and-survivors/understanding-your-response/fight-or-flight/#:~:text=The%20%27fight%20or%20flight%27%20response,fight%27%20or%20%27flight%27.
2. Ibid.
3. Ibid.
4. Ibid.
5. Carter, Christine. (2020 July 27). Seven Ways to Cope with Uncertainty. Greater Good Magazine: Science-Based Insights For A Meaningful Life, University of California, Berkely. Retrieved January 21, 2023 from https://greatergood.berkeley.edu/article/item/seven_ways_to_cope_with_uncertainty
6. Ibid.
7. Anxiety Canada (n.d.). Intolerance of Uncertainty. Anxiety Canada. Retrieved January 21, 2023 from https://www.anxietycanada.com/articles/intolerance-of-uncertainty/
8. Psychology Tools. (n.d.) Intolerance of Uncertainty. Psychological Tools. Retrieved January 21, 2023 from https://www.psychologytools.com/resource/intolerance-of-uncertainty/
9. Ibid.
10. Russo, Francine. (2022 February 14). The Personality Trait “Intolerance of Uncertainty” Causes Anguish during COVID.” Scientific American. Retrieved on January 21, 2023 from https://www.scientificamerican.com/article/the-personality-trait-intolerance-of-uncertainty-causes-anguish-during-covid/
11.The Wellness Society. (n.d.). How to Deal with Uncertainty: 6 Tips From a Psychologist. The Wellness Society. Retrieved January 21, 2023 from https://thewellnesssociety.org/how-to-deal-with-un…
Women’s Mental Health: Concerns, Barriers and Support
Women’s Mental Health: Concerns, Barriers and Support

Sex and gender interact with a variety of other determinants of health to influence our mental health. Despite efforts to focus on equality, gender bias continues to create complications that can take quite a toll on women’s mental health.
Social beliefs and cultural practices influence us, even before birth, and carry on throughout our lives as we grow and develop into adults. They help build our understanding of what we can enjoy and how we “should” act. Sometimes, however, they become barriers preventing women from seeking the support they need.
This article will look at women’s common mental health concerns and explore some of the distinct physiological factors that affect their health. We will also share available resources and treatment options.
Common mental health concerns for women
At the turn of the Millennium, the World Health Organization decided to update its inaugural Status of Women’s mental health study published in 1993. The new document included a prediction: that depression would become “the second most important cause of disease burden in the world by the year 2020.” (1) Researchers further stated that “women in developed and developing countries alike [were] almost twice as likely as men to experience depression.” (2) And they warned that, “violence and self-inflicted injuries” would “have special relevance for women’s mental health.” (3)
Today, just a few years beyond that forecast, women are experiencing mental health challenges that outpace available support. Researchers have continued to focus on profiling the unique differences around the kinds of mental health challenges women tend to experience most frequently. They’ve found that “women are more likely to be diagnosed with anxiety or depression, while men tend toward substance abuse or antisocial disorders.” (4) They have also validated that women and men exhibit various differences in symptoms. The symptoms women may experience are more likely:
- Internalizing disorders, where emotions aren’t shared and “typically results in withdrawal, loneliness, and depression,” is more common in women. Men tend to do the opposite, developing “substance abuse” and “antisocial problems” that see them “externalizing their emotions which leads to aggressive, impulsive, coercive and noncompliant behavior.” (5)
- Focusing on negative emotions and going over their problems more repeatedly than men do. It’s a gender-based difference that characterizes women’s experiences with depression, where they seem more vulnerable to becoming “stuck” instead of engaging in more active problem-solving. (6)
- Hormonal triggers certainly contribute to changes in women’s bodies, and they are often seen as a natural cause of both pre- and post-natal depression. But the truth is that they are not always at the root of issues. There are other genetic and biological factors also at play.
Reconsidering the influence of harmful gender-biased narratives related to hormones
Recalling common behavioural stereotypes about women’s bodily functions probably doesn’t take much thought. Many factors beyond an individual woman’s biology influence their mental health. Still, it’s harmful gender-biased viewpoints that continue to perpetuate unfair beliefs.
The Lancet, a highly respected medical journal, published a series of studies exposing how gender beliefs can influence women’s care.
- One study revealed that while women’s sex hormones and an impairment of their fight-flight-flee responses shaped their experiences with depression, there were other psychosocial factors at play. Women reported that things such as low self-esteem, experiences with body shaming, and relationship stressors such as violence and sexual abuse also contributed to their depression. (7)
- When looking at anxiety, trauma and stress-related mental health conditions, researchers hypothesized that biological differences made women more vulnerable. They investigated how monthly fluctuations of hormones such as estrogen and progesterone affected women’s thinking and behaviours but ignored any psychosocial influences. (8)
- We shouldn’t ignore societal expectations’ role in influencing women’s physical and mental health, especially regarding reproductive health issues related to infertility or fundamental reproductive rights. Pressures and stresses can lead women to feel that they have lost control and a sense of direction over their lives. Consider how categorially many other non-biological issues contribute to women’s poor health. There are economic, legal, and environmental influences, as well as poverty and inequality related to women’s wages, opportunities, and living conditions.
Social and cultural beliefs feed discrimination and bias against women trying to secure care
Social and cultural ideas about femininity and masculinity influence our thoughts and actions and impact situations they shouldn’t. (9) For example, it’s not uncommon for women to report incidents where they have not been taken seriously by physicians. One report shared findings of over 1000 women over the age of 16 who completed a survey in the province of British Columbia. Many women frequently reported the need to advocate for their health to obtain diagnostic exams and treatment because their symptoms and concerns have been dismissed, stigmatized, or attributed to incorrect diagnoses. (10) Many women shared that they initially didn’t “think their gender played a role in their care…when asked to share specifics about their experiences, [but] it became clear that being a woman did influence their treatment.” (11)
It isn’t wholly unexpected. Research focused exclusively on male subjects has provided information and influenced medical practices for decades. Excluding females has, in some cases, delayed understanding of drug interactions and their effects on female hormones and health conditions. (12) Dr. Alyson McGregor writes about what she believes to be a “flawed assumption” that medicine that “makes sense in a male body [also] must make sense in a female one.” (13)
Historically, misinformed attitudes and beliefs about menstrual cycles sometimes led to women being misdiagnosed for serious medical conditions. Alarmingly, however, women still report that these attitudes cloud their current-day healthcare experiences. One panel of physicians said that they’ve come across women in their practices that have experienced situations where “heart disease [was] labelled as anxiety, an autoimmune disorder [was] attributed to depression, [and] ovarian cysts [were] chalked up to ‘normal period pain.'” (14) Another study revealed that 51% of women felt that a physician “had diminished or overlooked their symptoms” (15)
There are also differences between treatment approaches for women’s and men’s mental health conditions that can be attributed to unconscious biases in medical care. Developing more awareness to identify and address these problems is a big step towards improving women’s health care in general, but also helping to deliver critical support to women who are experiencing serious mental health conditions.
What are some ways for women to cope with these concerns?
Providing clear examples and information about a wide range of situations helps advocacy groups in their quest to influence reforms. When women share their experiences, it can create a demand for policy changes. Here are some ways that women can take action:
- Be prepared when you meet with doctors. Have up-to-date lists of prescriptions, vitamins, and supplements, and note any allergies to ensure that doctors are working with complete information.
- Be bold and ask questions. If answers aren’t immediately available, physicians do leverage their networks to better understand your experiences and provide the best care options for you.
- Trust that you are the most in-tune and well-informed person about your body. Intuitively, we often can tell when something feels off. When you experience symptoms of something unusual, take action to get medical care and keep pushing for answers.
- Seek out local and national organizations that are working to understand and improve women’s healthcare experiences. A quick web search of “woman’s health advocacy” can often provide local and national contacts. By connecting with these groups, you might learn about medical trials or discover other ways to improve women’s health care, including offering financial donations.
- Ask for second opinions or consider switching physicians if you aren’t satisfied with your experience. The latter may be more challenging to orchestrate because of the corresponding problem of physician shortages.
Hospitals are also doing their part to change the face of women’s healthcare by introducing specialized nursing roles, such as Forensic Nurse Examiners (FNE). These roles exist so that women build their value and self-worth after experiencing violence and abuse. Working with an FNE can help women develop confidence about their treatments and mental health recovery from traumatic events.
What are some factors that affect women’s mental health?
Awareness of the unique differences associated with women’s mental health concerns is essential because these can shift as we age. Some of the most common factors that affect women include:
- Premenstrual Syndrome (PMS) results from hormone fluctuations during women’s monthly menstrual cycles. It can include a variety of symptoms, such as headaches, bloating and increased emotional sensitivity. Depression and anxiety can intensify the symptoms.
- Premenstrual Dysmorphic Disorder (PMDD)shares a similar group of symptoms to PMS; however, it differs because they are significantly worse. PMDD is characterized by “extreme mood swings, tension, irritability, and severe depression. ” In many cases, it affects personal and professional relationships and worsens around a woman’s period. (16)
- Pressures many women feel about achieving or maintaining an idealized body image or lifestyle that social media has influenced are often referred to as body dysmorphia. Women believe that they must conform to what they see online, and this can result in other serious complications, such as:
- Eating disorders
- Women comprise the majority of people with eating disorders, at 85-95% of those diagnosed with bulimia or anorexia nervosa. (17)
- Anxiety
- One study showed that approximately 10% more young women experience anxiety-related conditions than men. (18)
- Depression
- While up to 5% of the world’s population is affected by depression, women’s occurrence rate is double that of men. (19)
- Suicide
- Women attempt suicide 1.5 times more than men. (20)
- Eating disorders
What are some of the barriers that prevent women from seeking treatment to improve their mental health?
Race and culture
One study found that lack of access to mental health support and cultural stigmas prevent women from getting the help they need. In some cultures, women with mental health challenges face severe stigma. Other times, language barriers create problems. For example, some languages do not have words to describe someone experiencing mental health challenges. (21)
Female international students studying in North America face intense pressure to balance their studies, earn income, and adjust to new living situations. In some cases, while they may have gained more independence and responsibilities, they struggle with family and cultural obligations that they must also maintain. Many of these women who experience mental health challenges don’t know where to turn for help.
Age, education, and income
According to Mental Health Research Canada, women under 25 are “over-represented among those with high anxiety, stress and depression and are less likely to seek mental health support, citing an inability to pay or not having insurance coverage as barriers.” (22) The problem can be partly attributed to a shift in employment practices. Full-time roles are becoming more difficult to find as younger women struggle to break into their fields. As a result, they often start off taking low-wage, contract positions that rarely offer benefits. When they need specialized support and healthcare, sometimes the fees associated with these services become prohibitive when weighed against covering basic living expenses. Mental health issues will go unresolved and become increasingly more severe.
Urbanization
- Mental health treatment is only sometimes available in smaller communities, and people must travel to regional centres for expanded services. For example, in Canada’s far north, people face everyday challenges with general medical care, but even more so with the ease of obtaining mental health services. Many rural communities also find the availability to coordinate care and treatment with traditional Indigenous medicine quite challenging.
What are some resources available for women seeking mental health treatment?
While many local resources are available, we would like to profile some broad-based solutions that women may be interested in exploring.
If you live in Canada, visit the Government of Canada website and search for “Mental Health Support: Get Help” to find links to national and provincially-based services.
https://www.canada.ca/en/public-health/services/mental-health-services/mental-health-get-help.html
If you are in the United States, start with the US Government’s Women’s Health website
https://www.womenshealth.gov/mental-health/get-help-now
What can we do to support women and their mental health better?
There are some initial steps we can begin to take that will offer better support for women and improve their mental health:
- Acknowledge gender inequality.
- Ensure that women are better supported at home and in workplaces.
- Speak out against misinformation.
- Hold employers accountable for developing diversity, equity and inclusion policies that are respectful and inclusive for all women.
- Remember to act with kindness and compassion, always.
With encouragement, awareness, and increased availability of resources, women can develop better resilience and feel more supported.
References:
1. World Health Organization, (2000). Women’s Mental Health: An Evidence Based Review. Mental health Determinants and Populations Department of Mental Health and Substance Dependence, World Health Organization. Retrieved December 29, 2022 from https://apps.who.int/iris/bitstream/handle/10665/6…
2. Ibid.
3. Ibid.
4. American Psychological Association, (2011). Study Finds Sex Differences in Mental Health. American Psychological Association. Retrieved December 29, 2022 from https://www.apa.org/news/press/releases/2011/08/me…
5. Ibid.
6. Nolen-Hoeksema, 1987; Nolen-Hoeksema, Wisco, & Lyubomirksy, 2008, as cited by Eaton et. al, (2011). Brief Report: An Invariant Dimensional Liability Model of Gender Differences in Mental Disorder Prevalence: Evidence From a National Sample. Journal of Abnormal Psychology, American Psychological Association. Retrieved December 29, 2022 from https://www.apa.org/pubs/journals/releases/abn-121…
7. Riecher-Rössler, A. (14 November 2016). Sex and Gender differences in mental disorders. The Lancet Psychiatry. Retrieved December 29, 2022 from https://www.thelancet.com/journals/lanpsy/article/…30348-0/fulltext
8. Ibid.
9. Reviewed by Coveney, S (2022 January 31). The Gender Gap in Mental Health. News Medical Life Sciences. Retrieved December 29, 2022 from https://www.news-medical.net/health/The-Gender-Gap…
10. BC Women’s Health Foundation in partnership with Pacific Blue Cross (2019 October). In Her Words: Women’s Experience with the Healthcare System in British Columbia. BC Women’s Health Foundation. Retrieved January 10, 2023 from https://assets.bcwomensfoundation.org/2020/10/28162020/BCWHF-In-Her-Words-Report-2019.pdf
11. Furfaro, H. (2022 September 16). Why women with serious mental illness often get worse care than men. The Seattle Times. Retrieved December 29, 2022 from https://www.seattletimes.com/seattle-news/mental-h…
12. McLean Hospital, (2020, July 22). The Impact of Age and Gender on Mental Health. McLean Harvard Medical School Affiliate. Retrieved on December 29, 2022 from https://www.mcleanhospital.org/essential/impact-ag…
13. McGregor, A.J.,M.D. (2020 May 19). Sex Matters: How Male-Centric Medicine Endangers Women’s Health and What We Can Do About It. Hachette Book Group Inc. p.7. Retrieved December 29, 2022 from https://www.alysonmcgregormd.com/book
14. Northwell Health – Katz’s Institute for Women’s Health. (n.d.). Gaslighting in women’s health: No, it’s not just in your head. Northwell Health. Retrieved on December 29, 2022 from https://www.northwell.edu/katz-institute-for-women…
15. CBC News. (2019 October 10). Half of women in B.C. say doctors have played down their health concerns, report finds. CBC News. Retrieved December 29, 2022 from https://www.cbc.ca/news/canada/british-columbia/bc…
16. McLean Hospital, (2022, March 4). Understanding Mental Health Over A Woman’s Lifetime. McLean Harvard Medical School Affiliate. Retrieved on December 29, 2022 from https://www.mcleanhospital.org/essential/understan…
17. Cooper, S. (2022 June 13). Women’s Mental Health: Facts and Statistics. Innerbody.com. Retrieved December 29, 2022 from https://www.innerbody.com/womens-mental-health-fac…
18. Ibid.
19.Ibid.
20. Ibid.
21. Pasieka, C. (2022 April 10). Racialized women face significant barriers when seeking mental health care, study finds. CBC News. Retrieved December 29, 2022 from https://www.cbc.ca/news/canada/toronto/racialized-…
22. Canadian Mental Health Association (CMHA). (2022 October 25). CMHA testimony before FEWO: young women and girls mental health study. CMHA.ca. Retrieved December 29, 2022 from https://cmha.ca/news/cmha-testimony-before-fewo-yo…
Employee Fatigue, Isolation and Loneliness
Employee Fatigue, Isolation and Loneliness

Employee Fatigue
Many employees have transitioned to working remotely, whether that means working from a home office, or their kitchen table – employers and employees have had to adapt. Working from home and having endless access and connectivity to your work can lead to longer working hours, which may in turn, lead to burnout. Unable to partake in face to face meetings, as well as having limited social interactions with colleagues may have employees feeling isolated. Maintaining good communication with your co-workers is essential in combating fatigue and isolation, and promotes stronger remote work arrangements.
Here are a few considerations to make the work from home transition easier:
- Have a dedicated workspace
- Where possible, select a workspace with natural light
- Create a schedule
- Change out of your pajamas and get dressed for the day
- Maintain a healthy diet and hydrate
- Take breaks
It is imperative to emphasize the importance of taking breaks during your workday, even when working from home. It’s often a simple oversight, however, by-passing breaks may occur as you adjust to a new work environment. You may also justify additional work time in an effort to increase your perceived value and productivity. Think back to when you were at your physical workplace, you likely spent some time taking a break from your desk and catching up with co-workers during your lunch – you still need breaks from your home workspace. By taking breaks throughout your workday, you combat both fatigue and burnout. When stepping away from your computer screen or going for a brisk walk to get some fresh air – you give your eyes and mind a much-needed break. “Working at home begins to fail when individuals forgo breaks. In fact, not sticking to a schedule can have major implications for both productivity and mental and physical health.”(1) Also, try eating your lunch away from your screen.
Isolation
Whether you’re in quarantine because you have contracted the virus, or isolating to do your part in slowing the spread of COVID-19, being confined to your home with a decrease in social interactions can take a toll on your mental health. In a recent survey, it was found that “people are starting to feel the full effects of these practices: 54 percent of Canadians feel lonely or isolated.” (2) Having strategies that will help you cope during isolation is extremely important. Some tactics to try include:
- Create a daily routine. Keeping up with a routine will give you structure for your day.
- Stay informed, but limit your media intake to reputable sources.
- Stay active. Go for a walk or a bike ride, while maintaining physical distancing.
- Keep in touch. Call or video chat with your friends and family.
- Find a healthy distraction. Learn a new hobby or practice a skill you’ve been neglecting.
Loneliness
Everyone will experience loneliness differently, it is a personal experience. Some employees may not experience it at all, but others not accustomed to extended periods of time away from others, or those who covet social interactions may experience extreme feelings of loneliness. Regardless of your position, all feelings are valid. Remember you are not the only one feeling this way. “Now more than ever there is less reason to feel any shame or apprehension about loneliness; it may feel easier to share with others if you are finding it tough, and you are more likely to feel supported and understood by others.” (3) It can be helpful to address your needs with friends or family members as social support is a healthy way to stay connected. The feeling of loneliness may seem never-ending, so it’s important to stay connected to yourself and know your feelings are valid. Try meditation or journaling to reflect on how you’re feeling each day.
The Australian Psychological Society states that “we experience loneliness because it is a trigger for us to reach out and connect with others.” (4) Ensure you stay connected with your professional and personal networks. With the technological possibilities nowadays, there are many ways to stay in touch with people, regardless of where they are. Set up a weekly online video call, play virtual card or board games with friends or having a virtual family dinner can help you feel connected to your support system.
Self-Care
When what we have known as the “norm” is no longer relevant and there are so many drastic changes, it is important that we care for our mental health. One of the many ways to do so, is through self-care. The importance of “developing a healthy self-care practice means that you are willing to do some work to discover what makes you feel fulfilled. You’re also willing to try and achieve a better balance between your physical and mental health.” (5) Society has such a large impact on what we see as “ideal” self-care routines, but it is important to do what makes you feel good and fulfilled, as everyone’s self-care routine will look a bit different.
If you’re unsure where to get started, some very basic self-care tips include: getting enough sleep, eating healthy, exercising, limiting your screen time, and spending some time outside.
In addition to self-care, it is important to also practice self-compassion. Don’t resist your feelings of isolation or loneliness, but instead “find ways to be accepting of them as coming and going.” (6) We’re all in this together.
References:
- Collie, Meghan (2020). Source: https://globalnews.ca/news/6929809/coronavirus-wor…
- Collie, Meghan (2020). Source: https://globalnews.ca/news/6793214/coronavirus-can…
- Australian Psychological Society (2020). Source: https://www.psychology.org.au/getmedia/2612f989-02…
- Australian Psychological Society (2020). Source: https://www.psychology.org.au/getmedia/2612f989-02…
- Life Lines, Issue #07. Self-Care: Time and Attention for you
- Cuncic, Arlin (2020). Source: https://www.verywellmind.com/how-to-cope-with-lone…
Youth, Teens and Mental Health
Youth, Teens and Mental Health

Children And Mental Health Disorders
It’s no secret the emotions and actions of youth and teenagers can be a dizzying array of ups, downs, quirks and contradictions.
As adults, it may be difficult to imagine children suffering from such difficult challenges, yet child psychiatrist, Dr. Jean Clinton, worries the number of young people today experiencing mental health problems is on the rise. The statistics do paint a striking portrait: close to 20 percent – one in five – young people are actively dealing with a mental health issue. These include:
- Anxiety disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Bipolar disorder
- Conduct disorder
- Depression
- Eating disorders
- Psychosis
- Schizophrenia
- Suicide
Of these, anxiety disorders most commonly affect children and teens, with six percent experiencing them at some point. Suicide, the most concerning of mental health issues, is the number one non-accidental cause of death among Canadian youth. The Canadian Mental Health Association (CMHA) reported that a shocking five percent of youth attempted suicide in the past year, while another 12% had given suicide serious thought. Without question, our youth and teens are facing stressors and pressures in their lives which are manifesting in ways that go well beyond the often inconsequential “growing pains”.
Just as concerning, only one in four will get the help they need. This can create a disruptive ripple effect: the mental illness itself makes its way into the daily fabric, relationships, academics and physical health of the child. This, in turn, can negatively impact their future development, their overall mental and physical well-being and their perceptions of success in their adult lives.
It’s crucial that we eliminate the stigma and fear surrounding mental health, while opening up helpful dialogues that will benefit youth now and in the years to come.
Mental Health Disorders: What To Look For
With 50-70% of mental health disorders showing up before 18 years of age, it’s important to identify those who are struggling as early as possible. Some of the most common signs to watch for are:
- Avoiding people, places or situations they normally engage with or suddenly keeping to themselves
- Changes in eating patterns, feelings or behaviour surrounding food, weight or physical appearance
- Changes in self-esteem or self-image
- Changes or decline in relationships at school, home, or with other kids
- Changes or decline in school or extracurricular performance
- Changes or inability to sleep, relax or concentrate
- Deliberately hurting themselves or others
- Inability to cope with everyday life, issues or activities
- Lack of regard or interest in the feelings or property of others
- Lack of self-care or neglecting themselves
- New or increased use of alcohol and/or drugs
- New or unusual physical behaviours or ailments like recurring head or stomach aches, neck pain, excess energy or nervous habits (i.e.: nail biting, hair twisting, thumb-sucking, odd or repetitive movements)
- Overreactions to relatively small incidents
- Reduced interest in social or extracurricular activities they normally enjoy
- Speaking of suicide or having a preoccupation with death
- Sudden changes or extremes in emotion such as feeling rejected, worthless, hopeless, sad, helpless, anxious, worried, guilty/self-blaming, disillusioned, angry or afraid
- Sudden or unexplained changes in behaviour (i.e.: an active child becomes withdrawn or a good student’s grades drop)
Certain circumstances may also make children more susceptible to mental health disorders. These include:
- A family history of mental health disorders
- A history of previous suicide attempts
- Being gay, lesbian, bisexual or transgendered
- Ethnicity and societal discrimination
- Facing or having witnessed trauma, including abuse
- Having been the victim of, or having engaged in bullying
- Having recently gone through a major life change (moving to a new country, city or school)
- Having substance abuse problems
If you’re concerned about your child, talk to them about how they’re feeling. Letting them know you care is a powerful first step in showing they aren’t alone.
Ensuring Children Don’t Suffer Alone: Being Proactive and Offering Support
Daunting as it may be to broach the subject of mental health and kids, there’s reason to be optimistic: 70 per cent of mental health cases that appear in children can be addressed through early intervention.
Getting ahead of mental health disorders, and offering support to those who need it empowers both the at-risk child and the adults who love them. The good news? There are a multitude of ways to do just that.
Foster resiliency: As a parent, resist the urge to “bubble-wrap” or constantly protect your kids. Instead, actively provide the tools and skills to help your child problem solve, resolve conflict and help cope with the normal roadblocks, responsibilities and inevitable setbacks they’ll face. Boost their self-confidence by supporting good decision-making, assertiveness, perseverance and self-determination.
Communicate: Openly, honestly and often. Some of our favourite expert advice:
- Notice the little conversation openers your child offers up
- Ask non-judgemental questions and really pause to listen to what they have to say
- Acknowledge their feelings
- Answer questions directly and honestly
- Give your undivided attention
- Resist the urge to quickly jump in with solutions or advice
- And, above all, make time to connect whenever you can
Apart from keeping the lines of communication open and natural, checking in frequently also provides a great baseline; if things change where your child’s mental health is concerned, you’ll be far more likely to notice it, and they’ll be far more likely to share their struggles with you.
You and your child may also consider creating a signal (i.e.: a code word or specifically worded email or text message) to be used when they’d like to open a discussion about something important. This can help set the stage for a conversation they may not otherwise know how to begin.
Nurture a healthy, safe environment at home: Establishing routines and setting clear boundaries, rules and limits are key, as is building in daily time together. Mealtimes are fantastic opportunities to talk and listen (especially when devices are put away!). In fact, research suggests kids who share fewer meals at home with their family actually become sexually active or experiment with drugs at earlier ages, while kids living in a healthy, supportive environment have better mental health and less risk of mental health disorders.
Be respectful: Demonstrate that you value and accept your child for who they are.
Create a network of strong relationships: Help your child build a wider support system through friends, team sports, their church or other social activities. Even taking care of a pet can prove deeply fulfilling and beneficial to mental health.
Provide outlets to relieve anxiety and stress: Physical activity, meditation and the arts are super for self-expression, growth and work wonders on a young person’s overall mental health and ability to handle stress.
Avoid involving children in adult problems: When dealing with your own personal issues, look to other adults for support instead of bringing your child into the fray. Not arguing in front of your child or asking them to pick sides is important to ensuring your child’s mental health is maintained.
When necessary, seek professional help: If your child needs more intensive support, don’t hesitate. Your EFAP or family doctor are great places to start. They can help you navigate the various therapists, therapies, support groups, help lines and other services available, and determine which may be the best fit for your child. Provide information on your EFAP or local help line to your child so they can access services themselves, confidentially, if they ever need someone else to talk to.
Mental Health and Stability Outside the Home: Staying Informed About Your Child
Whether school, sports, work or their social lives, your child likely spends significant time away from the predictability of home. Be assured, however, that staying in the loop is possible, encouraged and supported by your community. You need only reach out or take some initiative to get a read on how your child’s doing outside the home. Consider:
Keeping an eye on online activity: Monitor your child’s social media activity or messaging apps to see how they’re feeling, coping and interacting with others. Keep it subtle and non-intrusive so your child feels their self-expression and privacy are being respected.
Communicating frequently with those who interact with your child: Teachers, guidance counsellors, administrators, friends, youth leaders and other parents can offer unique insights into how your child or teen may be acting or feeling when you’re not present.
Getting involved…together: Joining your child in activities they enjoy, or volunteering together for a good cause provides a space for bonding, self-esteem building, communication and connections that are often different than at home.
Mental health disorders in children and teens can be a source of great trepidation and fear, but it needn’t be. Acknowledging the very real challenges and complexities facing children – and letting them know you’re there to listen and help – this can be just what’s needed to ensure they feel supported, allowing them to flourish, during this exciting and dynamic time in their lives.
Recreational Therapy: Moving Toward Mental Health and Addiction Recovery
Recreational Therapy: Moving Toward Mental Health and Addiction Recovery

By learning to move their bodies in new ways, Canadians with mental health and addiction challenges are rediscovering their strength, resilience, and joy.
Walking in a park. Taking a moment to focus on your breath. Holding a yoga pose. These activities may seem simple — even frivolous. But they are part of a therapeutic approach that is transforming outcomes for people undergoing mental health and/or addiction treatment in Canada.
Recreational therapy improves physical, social, emotional, and cognitive functioning through leisure, recreation, and play. For people with mental health and addiction challenges, recreational therapy not only changes our bodies, but it also changes our brains on a chemical level. The result can be greater self-confidence, self-esteem, social connections, motivation, strength, and a sense of purpose — all of which support treatment and recovery.
The benefits have been proven through extensive research, and in 2016, the World Health Organization (WHO) officially recognized exercise as a proven therapy for mild to moderate depression and anxiety.
“We tend to separate ‘exercise’ from all the other ways we move our bodies, but it’s a continuum, and all movement is valuable.”
Recreational therapy is for everyone
Becoming and staying active isn’t always easy. Only one in five Canadians meet the recommended level of physical activity. People seeking mental health treatment in Canada for issues such as depression, anxiety, PTSD, or addiction often face even greater barriers to adopting an active lifestyle, including negative self-image, low energy, and physical health concerns.
In these cases, a recreational therapist can help the individual to overcome those barriers and incorporate movement and recreation into their mental health treatment options. A recreational therapist is a healthcare professional who helps individuals improve their physical, social, emotional, and cognitive functioning through recreational and leisure activities.
Chris Seftel, strength and conditioning coach at The Residence at Homewood, an inpatient treatment facility in Guelph, Ontario, says many of his clients mistakenly believe that this type of therapy is only for people who are young and fit.
“I work with a vast range of clients, from high-level athletes to sedentary desk workers, and from people in their twenties to people in their eighties,” says Seftel. “The exercises are tailored to each person’s abilities, needs, and preferences.”
Ronnie Birkland, recreational therapist at Homewood Ravensview, a private inpatient facility on Vancouver Island, British Columbia, agrees that this type of therapy is infinitely adaptable.
“We’re all at different stages in our lives,” he says. “We have different injuries, different backgrounds, and all of these things can make us feel intimidated. My job is to break that down and modify the activities so they don’t feel overwhelmed.”
“There’s a perception that recreational therapy has to be tough or intense, but it doesn’t. It doesn’t need to be hard. It doesn’t need to feel like work.”
How recreational therapy works
Recreational therapy is part of a holistic approach to mental health and addiction treatment. At The Residence at Homewood and and Homewood Ravensview, for example, the recreational therapist is an integral part of an assessment team that also includes an occupational therapist, dietician, nurse practitioner, social worker.
The recreational therapist works closely with the individual to build a foundation of trust, explore recreational options, and build a personalized program designed to deliver immediate and long-term benefits.
Building trust
Building trust between the client and the therapist is a big part of the process. People begin the journey to recovery at a very vulnerable point in their lives, and recreational therapy asks them to take a big leap of faith.
Birkland creates connections with his clients through empathy. “I’ve been through trying times myself,” he says. “I can tell them from my own experience, ‘This is what helped me. This is my blueprint.’ I allow myself to be real and let them feel that they’re in a safe place and that we’re in this together.”
Seftel builds trust with his clients by following a rigorous, evidence-based approach that conforms to recommendations set by organizations including the World Health Organization (WHO), Canadian Network for Mood and Anxiety Treatments (CANMAT), and the Canadian 24-Hour Movement Guidelines. Knowing that his methods are based on credible research reassures people who are putting their recovery in his hands.
Exploring the options
Working with the client one on one, the recreational therapist gets to know them closely — their background, goals, and concerns, the types of activities the client has participated in and enjoyed in the past, and the level of effort the client is willing or able to make as a starting point.
“There’s a perception that exercise has to be tough or intense, but it doesn’t,” says Seftel. “It doesn’t need to be hard. It doesn’t need to feel like work. I try to talk about ‘perceived exertion’ instead of ‘high intensity.’ For someone who has been almost immobile, high-intensity exercise could look like a three-minute walk. And that’s still therapeutic.”
Birkland agrees that the experience should be more uplifting than grueling.
“More often than not, there are things the individual loves to do, but they have not connected with them for years,” Birkland says. “They used to find joy in these activities, but that got taken from them at some point. Rediscovering that joy completes the healing process.”
“I’ve been through trying times myself. I can tell them from my own experience, ‘This is what helped me. This is my blueprint.'”
Creating a program
Seftel and Birkland both focus on designing recreational programs that align with the individual’s interests, preferences, and capabilities. Depending on these considerations, the program could begin with something as gentle as a five-minute walk three times a week or something more physically challenging, including hiking, running, swimming, weight or circuit training, yoga, or pickleball.
Over a period of weeks, the therapist helps the client set and achieve new movement and fitness goals so that they can see tangible progress and experience a sense of achievement.
Following through
Ultimately, the goal is to give the individual the tools they need to make recreation and exercise a permanent part of their lives. That means finding a program that fits their lifestyle, their location, their abilities, and their budget.
“When the 24/7 caregivers, doctors, and therapists aren’t there anymore, when they’re back in ‘real life,’ they have the tools they need to care for themselves and take control of their overall wellbeing,” says Birkland.
“People start to develop some self-compassion. Rather than ruminating on the mistakes they’ve made, they’re focusing on the positive things they’ve done, the things they’ve accomplished.”
The proven impact of recreational therapy
Extensive scientific evidence shows that exercise and movement have a measurable, positive impact on people with conditions such as depression, addiction, anxiety, and post-traumatic stress disorder (PTSD).
People with depression. Aerobic exercise and weightlifting have been shown to be effective in restoring neuroplasticity and reducing the symptoms of major depression. (Neuroplasticity is the ability of the brain to form and reorganize synaptic connections.)
People with addiction. Several studies suggest that exercise participation can reduce cravings, improve withdrawal symptoms, and reduce triggers in heavy cigarette smokers.
People with anxiety. Studies show that exercise is a viable treatment option for anxiety. Exercise increases the amount of a specific protein called brain-derived neurotrophic factor (BDNF) that protects and repairs the brain and reduces feelings of fear.
People with post-traumatic stress disorder (PTSD). Exercise decreases the activity of the sympathetic nervous system and hypothalamic-pituitary-adrenal (HPA) axis, which affect our physiological reactions to stress, including secondary conditions such as sleep apnea and migraines.
Vigorous exercise can also release natural “feel-good” chemicals such as endorphins and endocannabinoids (eCBs), which create feelings of euphoria (also known as a “runner’s high”). Research suggests that these good feelings can help to support sobriety and stave off or reduce the intensity of depression and anxiety.
Seftel says one of the earliest effects he notices is a change in energy levels for his clients. “People are amazed that after putting in the effort, they actually come away with more energy, not less. It’s this incredible sense of accomplishment.”
For Birkland, it’s the psychological changes that shine through. “People start to develop some self-compassion. Rather than ruminating on the mistakes they’ve made, they’re focusing on the positive things they’ve done, the things they’ve accomplished.”
Recreational therapy: Myths and realities
While modern therapeutic recreation has been in existence since the 1950s, it’s still not widely known in Canada as a treatment for mental health and addiction. Birkland and Seftel say it’s common for clients to feel apprehensive about starting a therapeutic program and exercise because of misinformation about this treatment modality.
These are some of the most common misunderstandings about recreational therapy and exercise.
Myth: Recreational therapy means hitting the gym.
Reality: You can move and improve anywhere. “People think of exercise as spandex and dumbbells and sweat,” Seftel says. “But there are hundreds of ways to incorporate movement into your day. Walk in your neighbourhood. Do yoga in your living room. There’s no wrong way to do it.”
Myth: Only high-intensity exercise is effective.
Reality: Any level of movement is beneficial. “Instead of ‘high intensity,’ I try to talk about ‘perceived exertion,'” says Seftel. “We tend to separate ‘exercise’ from all the other ways we move our bodies, but it’s a continuum, and all movement is valuable. Wherever you currently are is exactly where you need to be for us to start working forward.”
Myth: You need to meet a minimum fitness threshold.
Reality: People of any age or ability can participate. Research shows that people of all ages, abilities, and fitness levels benefit equally from recreational therapy. “There are always those blocks, that inner critic, the judgment inside,” says Birkland. “For so many, if they’re not good at it, they don’t want to try it. Throughout my time with them, I ask the questions that help them break down those barriers.”
“Motion creates motion”
For many people, recreational therapy starts small. But the impact is huge. Research shows that moving our bodies and pushing our physical limits — even just a little — can have a profound effect on our health and resilience. For people coping with mental health and addiction, this treatment can start a cascade of beneficial effects to aid recovery that go far beyond the physical.
“Recreational therapy opens so many doors in terms of the experiences you can have and the communities you can create,” says Seftel. “Movement is such a massive part of our lives, and motion creates motion.”
How Stigma Impacts Post-Traumatic Stress Treatment for First Responders
How Stigma Impacts Post-Traumatic Stress Treatment for First Responders

You’re the one who answers the call.
The one who shows up.
The one who offers light through life’s darkest moments.
So how could you possibly be the one feeling lost?
Feeling lost is common for First Responders, even while at work doing what they love.
If you’ve experienced feeling lost, at work or at home, you’re certainly not alone.
First Responders and Post-traumatic Stress
The Canadian Mental Health Association (CMHA) says First Responders (police, firefighters, and paramedics), military personnel, doctors, and nurses all experience higher rates of post-traumatic stress than people in other professions.
For example, twice as many First Responders compared to the average population experience a post-traumatic stress injury. That’s according to The Center for Suicide Prevention.
Dr. Jonathan Wan, MD, FRCP(C), Medical Director at Homewood Ravensview adds that this can look quite different from person to person.
General signs of post-traumatic stress, according to Dr. Wan and the CMHA, include:
- Anxiety, avoidance, and dread about attending work
- Insomnia and/or nightmares about traumatic events
- Feeling “on edge” and full of physical tension
- Apathy or having reduced interest or pleasure in spending time with others or engaging in usually enjoyable activities
- Persistent self-blame or guilt related to traumatic experiences
- Re-experiencing the traumatic event
- Feeling detached from reality or lost, disengaged, not really present
- Emotional numbness or having hard time feeling or expressing emotions
- Concentration issues (ie., brain fog)
Stigma Still Exists. You Can Fight Back.
“Unfortunately, stigma for First Responders reaching out still exists today,” says Steve Farina, City of Coquitlam Fire Captain, Vice President of Lower Mainland North at BC Professional Fire Fighters Association and Vice-Chair of the BCPFFA’s Mental Health Taskforce and Occupational Health & Safety Committee.
Stigma can be internal (ie., self-stigma) or external (ie., from peers or institutions).
Internal stigma
“The biggest barrier for reaching out seems to be self-stigma (that internal conversation where one feels weak, fearful of being judged, etc.),” says Farina.
Dr. Wan further explains that despite greater awareness related to mental health issues, reaching out can still remain difficult.
“Part of the reason is because internalized stigma can present as the negative attitudes and self-judgement we have about our own experiences,” he says.
External stigma
External stigma can come from comments said by colleagues and supervisors, or fears about what they may say or think.
Negative perceptions (ie., judgements) and harmful behaviours such as gossip towards First Responders who have experienced mental health challenges or mental health conditions are examples of external stigma, says Farina.
Dr. Wan adds that external pressures can range from peers looking unfavorably on taking time away for recovery to institutions not acknowledging the impacts of psychological injuries.
“Whatever the source, stigma can compound mental health difficulties and prevent individuals who would benefit from treatment in seeking prompt care,” he says.
Expert Advice for First Responders
Farina says his advice for any new First Responder beginning their career is to connect to a mental health professional right away.
While we understand it’s not always easy to reach out, Farina suggests there’s benefit to seeking support sooner than later.
For First Responders with post-traumatic stress injury diagnoses, the accumulation of psychological injuries in the workplace at the expense of one’s health seems to be a common occurrence, he explains.
It’s vital for First Responders to understand their health and act accordingly, adds Wan.
“The saying of putting your own oxygen mask on in a plane before helping others is a fitting analogy,” says Dr. Wan.
“Don’t wait until your backpack is full of traumatic calls and stress and you’re overwhelmed, burned out, etc.,” he says.
Farina’s suggestions:
- Find a mental health professional you can trust and relate to
- Establish a relationship and baseline history early in your career
- Check-in regularly throughout your career
Leaving symptoms of post-traumatic stress untreated can build up into a traumatic stress injury or diagnosis of PTSD.
“PTSD usually appears within three months of a traumatic event, but sometimes symptoms may not appear for years,” according to the Canadian Mental Health Association.
The benefits of working with someone at any time, according to Farina, include learning tools to:
- Destress
- Down-regulate your nervous system
- Develop the awareness to know when to take a knee and reach out for help or additional support
If you’re already experiencing early signs and symptoms of post-traumatic stress, Farina encourages you to reach out and tell your supervisor, spouse, trusted coworker, or friend.
The Homewood Ravensview Difference
Come home to yourself at Homewood Ravensview.
Since opening in 2019, we’ve helped over 400 First Responders find their path forward from post-traumatic stress injuries.
We’ve made it part of our mission to continue learning and developing programming specific to the unique needs of this critical group. We do this by learning from people who get it because they have experienced something similar and know that while every trauma experience is different, you can heal from this injury, too.
Continual Learning
In partnership with Wounded Warriors Canada, Homewood Ravensview employees were given access to specialized occupational awareness training for the treatment of trauma-exposed professionals such as members of the Canadian Armed Forces (CAF), veterans, and other First Responders (ie., police, fire, emergency service professionals, etc).
The Introduction to Trauma-Exposed Professionals training program, developed by Wounded Warriors Canada’s co-National Clinical Advisor, Dr. Tim Black, has been designed to help increase competencies in the divide that exists between trauma-exposed professionals and the public.
The training program provides culturally-specific clinical approaches to support the complex mental health needs of trauma-exposed professionals and, through our partnership, is available to all Homewood Health employees.
Healing Outside of the Uniform: Guardians Program
The Guardians program at Ravensview supports First Responders in their journey in recovery from mental health difficulties.
Highlights of Treatment
- Personalized for your unique needs
- Medication consultation and management
- Access to group and individual therapy
- Ongoing assistance from trained professionals
- Peer support from other First Responders
Treatment starts with a comprehensive and multi-disciplinary assessment to better clarify your individual needs.
You’ll gain access to individual and group talk therapy and educational tools about psychology to support your overall wellness needs.
A diverse team of physicians will then discuss ongoing interventions that can include, but are certainly not limited to, medication management.
You’ll be involved in the process of your own medical care and get the support you, too, deserve.
According to Dr. Wan, every type of treatment occurs in a therapeutic setting with other First Responders. We’ve found this promotes safety and acceptance.
Homewood Ravensview believes in the transformative power of care because we’ve seen it firsthand. If you or someone you love feels lost from trauma or PTSD, take the first step – reach out. The courage to do so could be the beginning of your path forward.
Resources
- Canadian Mental Health Association. Post-traumatic Stress Disorder.
- Steve Farina, City of Coquitlam Fire Captain, Vice President of Lower Mainland North at BC Professional Fire Fighters Association and vice-chair of the BCPFFA’s Mental Health Taskforce and Occupational Health & Safety Committee.
- Dr. Jonathan Wan, MD, FRCP(C), Medical Director at Homewood Ravensview.
- The Center for Suicide Prevention. First Responders, Trauma & Suicide.
- BC First Responders Mental Health
The Link Between Doom Scrolling and Young Adult Mental Health
The Link Between Doom Scrolling and Young Adult Mental Health

We live in an increasingly digital world, and we know it’s impacting and influencing our mental health.
Pre-pandemic data from the Canadian Internet Survey reported by Stats Canada suggests social media use negatively affects everything from our sleeping habits to how much physical activity we get and how well we can concentrate on everyday tasks.
According to the report, one in eight or 12-14% of social media users also reported feeling:
- Anxiety
- Depression
- Frustration
- Anger
- Envy by comparison (ie., scrolling and seeing other people’s lives on social media creates feelings of envy)
“Many young people report being online with friends, family and others almost constantly . . . but some young people’s online behaviours have had such an effect on their lives that they have been labelled as ‘problematic,’ according to the Government of Canada’s findings from the 2018 Health Behaviour in School-aged Children (HBSC) Study.
If this resonates with you or someone you care about, you’re certainly not alone.
“Social media, in particular, has become a key source of news and information over the past few years,” says Dr. Monica Vermani, Clinical Psychologist and Author of A Deeper Wellness: Conquering Stress, Mood, Anxiety and Trauma.
The trouble is that “social media is a largely unregulated platform, rife with over-stated, unsubstantiated, unreliable, and highly questionable news sites that rely on attention-grabbing, sensationalizing, and fear-mongering tactics that employ pseudoscience, conspiracy theories, and highly manipulative misinformation to generate traffic and ‘clicks’ that monetize their online businesses,” she explains.
“This relentless exposure to negative stimuli fuels negativity, fear, and self-doubt, and hijacks and overwhelms habitual users’ critical thinking abilities,” she adds.
Young Adults Deserve More Than a Side of Anxiety and Depression with their Connections
For young adults, it’s arguable that increased accessibility and acceptability of social media use has worked to increase social connections.
But online connections may not be a suitable or sustainable replacement for real world experiences during this critical life stage. What’s more, they may be contributing to anxiety and depression.
“Young adults are in a state of transitioning into full adulthood, a process that involves distancing somewhat from their family of origin and establishing themselves in intimate-partner relationships, living on their own for the first time, and pursuing careers,” says Dr. Vermani.
“At this stage in life, building strong social networks and relationships with others is crucial to their sense of self and connection to the world,” she adds.
Unfortunately, problematic social media use has been associated with anxiety, depression, and weaker relationships and connections, according to the HBSC study report.
How Social Media Contributes to Feelings of Depression and Anxiety
“What we focus on expands, and this includes exposure to and habitual consumption of the negative messaging that has expanded since the start of the pandemic,” says Dr. Vermani.
How the social media and negative news consumption cycle exists, according to Dr. Vermani:
- Social media feeds negative thoughts
Social media feeds negative thoughts or anxiety by reinforcing and perpetuating them. Dr. Vermani says social media-influenced negative thoughts, beliefs, and mindsets can significantly impact consumers’ mental health and exacerbate symptoms of depression or anxiety. - Social media fuels negative thoughts
Social media fuels negative thoughts by adding gas to the fire of dread, worry, fear, stress, anxiety, hopelessness, and depression that lead to catastrophizing worse-case scenarios, panic attacks, or suicidal ideations for those with anxiety and depression. - Social media can make existing mental health conditions like anxiety and depression worse
Dr. Vermani explains that increasing habitual doom scrolling negatively impacts sleep, worsens mood-based symptoms, and leads to lower productivity, decreased mental acuity, and ability to deal with real-life stressors and responsibilities over time.
Healthy Consumption: How Much Media Is Too Much Media?
Too much of a good thing is bad news, and social media is no exception.
Dr. Vermani says that regardless of the quality of media consumption, too much time on media of any kind — including social media — is linked to feelings of depression and low self-esteem.
This happens, she explains, “often as a result of self-judgment, as a result of over-exposure to the unreal and/or unrealistic standards and facades perpetuated on all forms of media and social media.”
She adds that frequent or obsessive use of screens can:
- Exacerbate feelings of disconnection and loneliness (ie., feeling lost).
- Increase physical or mental isolation as screen use is largely a solitary endeavor that drains energy and steals time viewers/users would typically spend connecting with friends and/or family members.
- Lead to social anxiety (fear of scrutiny, judgment, and evaluation) and social unease or awkwardness.
“Exposure to fear-inducing headlines, conspiracy-based content, and apocalyptic forecasting triggers the fight-or-flight response, in particular, which sets off a continual stream of cortisol — the stress hormone,” she explains.
While cortisol is fine in small doses, over time, the brain and body become exhausted by the high levels of this stress hormone, she adds.
“This contributes to a host of medical problems (including immune system function, digestive issues, weight gain, blood sugar levels, and heart disease) as well as mental health issues and cognitive impairment,” says Dr. Vermani.
The University of British Columbia confirms that excess cortisol in the blood can cause a variety of symptoms, “including high blood pressure, weight gain, thinning of the skin, easy bruising, poor wound healing and many others (sometimes referred to as Cushing’s syndrome).” Unmanaged overtime, this can lead to adrenal disorders and deeper health complications.
Signs It’s Time to Seek Support
Warning signs that social media consumption is becoming problematic include:
- Increased procrastination around life tasks and responsibilities
- Relentless need for stimulation (with anxiety, agitation, and boredom when away from screens)
- Obsession with negative cycling through current events even when performing or engaging in other tasks or social situations
- Mindless consumption of media
- Obsessive preoccupation with creating and sharing online content
- Guilt and shame of ‘time-wasting’ when on social media for over two hours per day
- Conflict with a partner, parents, friends, and/or an employer
- Diminished self-esteem due to a failure to measure up to the unrealistic lifestyle, financial and beauty standards portrayed on social media
- Increased fear of missing out (FOMO)
- Neglect around self-care, exercise, relationships, and hobbies due to time spent on social media
Tips for Building Emotional Resilience Against Negative Effects of Social Media
“It’s important that individuals in this age group take steps to build resilience to the negative impacts of over-exposure to doom-and-gloom social media and traditional media,” Dr. Vermani recommends.
This requires first recognizing when you’re engaging in catastrophizing, and working to challenge the likelihood or actuality of worst-case-scenarios taking place, and then examining and reframing negative thoughts.
Here’s what this looks like in more detail.
- Build awareness around the number of hours per day you spend on screens, media, and social media
- Tune-in to how a sensationalized article makes you feel
- Admit when technology use has become problematic
- Commit to change by limiting message checking and screen time
- Take a break from social media to help restore balance and perspective
- Start a buddy system to help with accountability
- Practice thought-stopping (a cognitive-behavioral technique used for ending obsessive or anxious thoughts).
- Try this: The next time you have difficulty turning off a negative thought, simply imagine a red stop sign. The power of engaging your imagination works to help curb negative thinking and rumination, says Dr. Vermani.
- Create mindful moments by briefly disengaging from screens to reconnect with themselves through breath or movement.
- Limit engagement in social media to when daily life tasks, responsibilities, and goals are complete
- Stay focused on the here and now. Making sure the here and now involves spending time doing things that bring us joy will keep us grounded in the world around us, and actively engaged in life, adds Dr. Vermani.
- Use positive affirmations, mantras, life-affirming sayings, and slogans that act as touchstones and reminders of the good in the world, other people, and ourselves
- Seek help to gain control of problematic habits and negative impacts related to over-exposure to screens and media when they cannot do so alone.
Dr. Vermani says when mood, anxiety, and self-esteem are negatively impacted by social media exposure, a primary care physician or family doctor is a great first step to accessing treatment options.
“People with mood, anxiety, and attention disorders often rely on self-soothing by scrolling on devices to alleviate symptoms of anxiety or distract from uncomfortable feelings. A mental health professional can help address the underlying cause of such problematic behaviors,” she says.
When You Need More Support: The My Path Young Adults Program at Ravensview
When social media or negative news consumption feels like it’s become all but too much or you’re not seeing results when changing behaviours, please bear in mind there are other options for support.
The My Path inpatient treatment program was designed with evidence-based programming, including group programming with other clients who are working on similar issues, so you can access real-world, in-person connections to others in your age group and professionals trained to understand behavioural compulsions, obsessions, and addictions.
We See Your Story as Unique
Our multi-pronged approach to fostering and establishing healthy connections and mental wellness in young adulthood means you’ll access treatment that acknowledges your uniqueness and supports you long-term.
You Should Know…
You don’t have to get sucked into the social media cycle of negative thoughts, anxiety, depression, or worse. You can learn how to cope with negative news and social media comparisons, navigate online relationships,and how to unplug for your overall mental and physical well being.
The My Path program is specifically and strategically designed for adults aged 19-25 years from all cultural and social backgrounds.
Our dedicated team of multidisciplinary professionals recognizes excessive or problematic social media use as another behavioural addiction similar to gaming and gambling. We also understand that you may be engaging in these types of behaviours as a means of coping.
We treat problematic use of technology as a symptom and we help you get to the cause of why you’re engaging in these behaviours in the first place.
While everyone’s story is unique, connecting with others in these in-patient community-based groups offers opportunities for developing the life-changing connections social media just can’t replicate or compete with.
Our expert staff are also equipped to support you with life stage challenges at the same time including, but not confined to, transitioning to adulthood, and questions around sexuality, identity, self-esteem, and social dynamics.
To learn more about what the My Path program can provide, please go to: https://ravensview.com/programs/young-adults/
Resources
- Stats Canada. Canadians’ Assessments of Social Media in Their Lives.
- Monica Vermani, clinical psychologist and author of A Deeper Wellness: Conquering Stress, Mood, Anxiety and Traumas. Personal interview. December 2022.
- University of British Columbia. Adrenal Disorders.
Post Holiday Blues: Is It Normal to Feel Sad After the Holidays?
Post Holiday Blues: Is It Normal to Feel Sad After the Holidays?

What are the post-holiday blues?
Post-holiday blues are different from depression. They are temporary feelings of sadness and anxiety. These feelings can begin as the celebrations and events of the season wind down and as routines return to normal.
After a short adjustment period, the post-holiday blues typically resolve on their own and people begin to stress less. This isn’t always the case, though.
Sometimes returning to regular programming after being in holiday or vacation mode can be more challenging than anticipated.
Facing difficulties in getting back to a regular schedule may contribute to feeling disconnected or lost.
Experts say signs of declining mental health or depression to watch for include:
● Less energy and changes to sleep patterns
● Less motivation or interest
● Less connection or increased self isolation
● Feeling lost and lonely
● Irregular eating behaviours, such as over- or under-eating
● Excessive worry and/or feelings of hopelessness
● Feeling compelled to or self-medicating with alcohol, drugs, or other substances/activities
● Thoughts of self-harm
Post-Holiday Stress and Mental Health Risks
While stress is a normal, everyday part of life, it becomes a potential problem when we have less support and coping tools than necessary to manage in a healthy way.
Without healthy coping strategies, anxiety and depression can build. Dr. Josh Hamilton, a psychiatric nurse practitioner and the Assistant Vice President & Dean of Post-Licensure Programs at Rasmussen University explains it’s not uncommon for people to turn to drugs and alcohol for any form of temporary relief during this life stage.
This is considered self-medicating. Rather than actually help you or someone you love stress less, though, drugs and alcohol can seriously worsen the symptoms they initially helped to briefly relieve.
If you’ve turned to drugs or alcohol to try to avoid feeling lost, or to cope with anxiety and depression, you’re certainly not alone.
Research suggests substance use disorders (including substance misuse, abuse, and dependence) tend to begin in early adulthood and continue into later life stages if left untreated.
It’s estimated that over 20% of Canadians will face troubles with problematic substance use during their lifetime.
Top four substances of use:
● Alcohol
● Nicotine (tobacco)
● Cannabis
● Opioids
The Dangers of Self-Medicating
If you’re trying to stress less, self-medicating isn’t a safe solution. There are short term risks with alcohol use. These include anxiety, depression, and suicide.
If you or someone you know is experiencing suicidal thoughts, please reach out today for help.
Talk Suicide Canada is available 24/7.
Text message (SMS) 45645 or call toll-free 1-833-346-4566
If you are someone you know is in immediate crisis, dial 9-1-1.
Post-Holiday Blues or Anxiety and Depression?
Hamilton highlights how important environmental or relational context is when making sense of how we feel, too. Knowing the difference between post-holiday blues and a clinical disorder like anxiety, depression, PTSD, or behavioural addiction can help you or a loved one determine when to seek support.
It’s also crucial to consider how the past few pandemic years may have had a cumulative effect, and contributed to feeling lost.
What may have been cause for concern pre-pandemic, such as feeling lost in general, says Hamilton, is more understandable after what we’ve been through the past several years.
Questions to Ask
Answering these questions for yourself or someone you care about can help provide some perspective on whether you’re dealing with post-holiday blues or something more serious.
For example, are you feeling lost in life because you’re not sure if you’re on the right relationship track; if you want to have children; or if you’re in the right career, or, are you experiencing feeling lost when spending time with people (ie., feeling alone in a room full of people)?
Hamilton explains while some specific scenarios of feeling lost are to be entirely expected, other more general feelings may be cause for clinical consultation with a healthcare provider or mental health professional.
You can also try asking whether or not your feelings are associated with actually being alone during this season or if it’s a larger life stage issue.
More questions to ask:
● How do you feel when reflecting back on the whole year (not just the past holiday season)?
● Is there a particular trigger (person, place, thing) causing these feelings?
● Can you explain how you feel?
By taking some time in the post-holiday period to reflect, you gain some control or at least an awareness of where feeling lost might be coming from.
Finding Relief During Darker Days
The literal darkness of the winter and holiday season doesn’t help matters much, either.
Hamilton explains the shorter days, earlier nightfall, and colder temperatures take a toll on our collective mental health.
We can of course support our wellness during this season by focusing on nutrition, sleep, physical activity, and remaining as social as possible.
“To help alleviate symptoms of stress, pessimism, or melancholy that often come with feeling lost, lean into self-compassion and embrace progress over perfection. There’s no rush to get to some end destination. True joy is found in enjoying the journey,” says Jhas.
Beyond the Benefits of Connection
Hamilton highlights the power of connection in healing from feeling lost.
He says asking for help may begin by telling friends and family how you’re feeling or reaching out to a mental health professional.
If you feel you may benefit from additional support, or are not getting what you need to cope with anxiety and depression, there should be no shame in seeking a deeper level of support.
“It’s like returning to your doctor with a cough that won’t go away,” says Hamilton. This should not feel embarrassing, but it’s understandable due to stigma if you feel nervous bringing up symptoms that aren’t resolving.
“Have a conversation to explore what’s going on with you,” suggests Hamilton. This conversation can take place with your primary care provider or with a private provider.
True to Homewood Health’s legacy, Ravensview’s Cornerstone program takes an interdisciplinary and holistic approach to treatment to accommodate the full spectrum of adult needs including physical, mental, social, and spiritual health.
We understand the unique difficulties people may face during this time of year, and we are here to help.
Contact us today at 1-866-203-1793 or reach out online.
Resources:
Aderibigbe, O. O., Stewart, S. L., Hirdes, J. P., & Perlman, C. (2022). Substance Use among Youth in Community and Residential Mental Health Care Facilities in Ontario, Canada. International journal of environmental research and public health, 19(3), 1731. https://doi.org/10.3390/ijerph19031731
Addiction Guide. Canadian Statistics.
Canadian Centre on Substance Use and Addiction. Alcohol.
Hamilton, Josh. Personal Interview. December 2022.
Jhas, Sonia. Personal Interview. December 2022.
Introduction to Cognitive Behavioural Therapy (CBT)
Introduction to Cognitive Behavioural Therapy (CBT)

Introduction to Cognitive Behavioural Therapy (CBT)
Many people find it fairly easy to think of ways that they can work on improving their physical health. For example, you might go for a walk, listen to your favourite music to make tackling house chores more enjoyable, or even head out to exercise classes. They’re all great ways to stay active and can help you realize benefits through an improved outlook on life and well-being. But when it comes to getting the equivalent “exercise” to improve your mental health, it can be trickier to understand what’s available and what will give you good results.
Cognitive Behavioural Therapy (CBT) is one of many proven therapy techniques. It can help us understand how negative patterns of thinking we have developed throughout our lives make us feel deflated, limited and more fretful. It can help us conquer self-criticism, feeling undervalued, anxiety, depression, low self-esteem, and other common mental health challenges. CBT focuses on identifying negative thought patterns that can often sabotage us and, instead, framing those thoughts differently to unblock our potential and find clarity. After a few sessions with clinicians or online modules, we can become more mindful of our thinking as we learn to embrace different CBT tools.
In this article, we’ll introduce you to some of the principles of Cognitive Behavioural Therapy and help you determine if it might be a type of therapy that you want to try. While it’s not the only type of therapy that can make a difference, it can be a great place to start when you want to work on improving your mental health.
What is Cognitive Behavioural Therapy?
Cognitive Behavioural Therapy (CBT) is a structured and collaborative form of “psychological treatment that…[often] leads to significant improvement in functioning and quality of life.”[1] It helps people recognize when their thinking patterns are distorted and may be contributing to the problems they are experiencing in their lives.
CBT is founded on the core principles that “psychological problems are based, in part, on faulty or unhelpful ways of thinking [and]…learned patterns of unhelpful behaviour.”[2] Additionally, this type of therapy helps people learn “better ways of coping” with their problems so that they become “more effective in their lives.” [3]
CBT helps people move forward from their current difficulties by developing better coping strategies. Working through some history is part of the therapy, but the main focus is to “make sense of what is happening around them and [see how their] perceptions affect the way they feel.”[4]
Why is CBT used?
CBT is a form of therapy because it helps address the thoughts people can get caught up in. Over time, this can affect someone’s outlook on life, making them feel more vulnerable. The methods and exercises we can learn through CBT show us that instead of feeling like we don’t have much influence over the directions our lives are taking, we can modify our thoughts and control how we react to situations. Practicing CBT can change how we feel about daily experiences and problems.
Psychiatrist Aaron Beck developed a model for CBT in 1976. It captured how we “think about things and the content of these thoughts.”[5] Beck’s model expresses three aspects of our thinking and their interrelationship to show how we build negative beliefs:
CBT is also practical because it is structured and time-limited. People usually attend between 6 and 20 one-hour-long sessions on a regular basis where they focus on a specific problem and work toward achieving specific goals that are agreed to at the start of the therapy.[7] In their sessions, people often feel more engaged in working through their issues because they begin to understand their negative thinking patterns and accept accountability for them. It’s a self-managed way to see how negative thinking influences their behaviour and vice versa: situations trigger automatic thoughts that affect core beliefs. It is also flexible enough to deliver in person, online or through mobile apps.
What is the goal of CBT?
CBT intends to equip someone with a set of practical tools they can use to assess situations they find themselves in that are leading to negative thinking. Some of these tools include:
- Setting SMART (specific, measurable, achievable, realistic, and time-limited) goals can help establish priorities to focus on. Working through and completing small goals helps by building momentum. You get a sense of satisfaction as you achieve things you may have thought impossible.[8]
- Learning to question assumptions and talk through situations with yourself will help you recognize self-criticism. You’ll also learn techniques to “name” what is happening to you when you begin to create “cognitive distortions.” You’ll be able to replace those negative thoughts with constructive ones to be kinder to yourself.”[9]
- Recognizing and learning to modify cognitive distortions. Cognitive distortions create harmful and destructive thinking patterns, which include: jumping to conclusions, always assuming the worst, all -or-nothing thing, always having to be correct, emotional reasoning, blaming, and focusing on what we believe we should have done.[10]
- Keeping a record of your thoughts. People can use tools such as journaling to help identify their negative thoughts and note positive replacements.[11]
- Rewards and incentives focus on creating activities that will improve someone’s overall positivity and mood. [12]
- Situation exposure is a technique used in cognitive behavioural therapy (CBT) to help people identify their fears and approach these fears in a safe, planned and deliberate way. It involves gradually exposing a person to a situation or stimulus that triggers feelings of fear or panic, in a safe space without the intention to cause any danger to the person. Over time, controlled exposure to these fears can help reduce the intensity of anxious or distressing feelings. For example, this tool can give new hope to people suffering from nightmares. Exposure to the situations that create the sense of panic they experience during a nightmare will help them learn that these sensations are not dangerous.[13]
- Mindfulness and relaxation/calming techniques such as deep breathing and muscle relaxation or body scans can help someone develop coping skills to help manage stressful situations and emotions.[14]
Who can benefit from CBT?
Everyone can benefit from CBT. It uses methods like working to understand thoughts and behaviours, using problem-solving skills and increasing confidence. Practicing these will produce changes that are “as effective as, or more effective than, other forms of psychological therapy or psychiatric medications.”[15]
One study revealed that after 5-15 CBT sessions, 50-75% of respondents with social anxiety said that CBT was highly effective.[16] Another series of studies found that when CBT and drug therapy were combined, the results were “superior for major depression, panic disorder and obsessive-compulsive disorder (OCD).”[17]
CBT treatment is effective for various situations, including: bipolar, depression, anxiety, panic attacks, phobias, substance use, PTSD, eating disorders, anger/aggression, relationship problems, trauma, pain, sleep problems, time management challenges, and general or situational stressors.
What to expect in your first CBT session
If you want to explore working with a therapist, your first meeting is a chance to determine how CBT can help you. You will also get a sense of whether you and this therapist have a good fit and can work together.
Here’s what might happen:
- You will determine your preference for a meeting (in person, online, or by phone).
- Your therapist will want to understand why you reached out for help and learn more about your work and personal lives.
- You might discuss costs and time frames/duration of sessions and whether you have coverage under a benefits plan.
- You should discuss the therapist’s background, training, and education.
- Your therapist will review their policy concerning confidentiality.
- Your therapist may ask you what your goals are for therapy so that you can develop a treatment plan together.
- You can discuss how you feel about homework and practicing CBT tools and ask any questions that you may have.
CBT resources
There are many CBT therapy resources available online that you can explore. We’ve included links to a few that you may find helpful. Remember that while CBT has a sizeable self-directed component, it’s always a good idea to consider working with a therapist. They can guide you through the processes and tools so that you understand how it works.
- Thought record worksheet
https://positive.b-cdn.net/wp-content/uploads/2018/01/Thought-Record-Worksheet.pdf
- Accepting Uncertainty Worksheet
- Postponing Your Worries
- Fact-checking thoughts worksheet
https://positive.b-cdn.net/wp-content/uploads/2020/09/Fact-Checking-Thoughts-Worksheet.pdf
- Functional Analysis worksheet
https://positive.b-cdn.net/wp-content/uploads/2020/09/ABC-Functional-Analysis-Worksheet.pdf
What if CBT doesn’t seem like the right fit?
If CBT doesn’t seem right for you, there are alternative therapy options that you can explore such as:
- Behavioural Therapy
There are many other types of behavioural therapy besides CBT. Which one is used depends upon the situation.
- DBT – Dialectical Behavioural Therapy
- Social Learning Theory
- Humanistic Therapy
It focuses on “a person’s individual nature rather than assuming a group of people with similar characteristics have the same concerns.”[18]
- EMDR – Eye Movement Desensitization Therapy
EMDR is used to reduce emotional distress from Post-Traumatic Stress (PTSD).
References:
[1] American Psychological Association (2022). What is Cognitive Behavioral Therapy? APA. Retrieved November 2, 2022 from https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
[2] Ibid.
[3] Ibid
[4] Canadian Association for Mental Health (CAMH) (2022). Cognitive behavioural therapy. camh. Retrieved November 2, 2022 from https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/cognitive-behavioural-therapy
[5] Fenn and Byrne (2013). The key principles of cognitive behavioural therapy. Sage Journals: InnovAiT Volume 6, Issue 9, September 2013, Pages 579-585. Retrieved on November 2, 2022 from https://doi.org/10.1177/1755738012471029
[6] Ibid.
[7] Canadian Association for Mental Health (CAMH) (2022). Cognitive behavioural therapy. camh. Retrieved November 2, 2022 from https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/cognitive-behavioural-therapy
[8] Raypole and Marcin (Medically reviewed by Lener, M. MD) (2022, May 17). Cognitive Behavioral Therapy: What Is It and How Does It Work? Healthline. Retrieved November 2, 2022 from https://www.healthline.com/health/cognitive-behavioral-therapy
[9] Ibid.
[10] Riopel, Leslie (2019, June 15). Benefits of CBT: 8+ Results of Cognitive Behavioral Therapy. Positive Psychology.com. Retrieved November 2, 2022 from https://positivepsychology.com/benefits-of-cbt/#:~:text=In%20particular%2C%20the%20strongest%20support,et%20al.%2C%202012).
[11] Raypole and Marcin (Medically reviewed by Lener, M. MD) (2022, May 17). Cognitive Behavioral Therapy: What Is It and How Does It Work? Healthline. Retrieved November 2, 2022 from https://www.healthline.com/health/cognitive-behavioral-therapy
[12] Ibid.
[13] Riopel, Leslie (2019, June 15). Benefits of CBT: 8+ Results of Cognitive Behavioral Therapy. Positive Psychology.com. Retrieved November 2, 2022 from https://positivepsychology.com/benefits-of-cbt/#:~:text=In%20particular%2C%20the%20strongest%20support,et%20al.%2C%202012).
[14] Ibid.
[15] American Psychological Association (2022). What is Cognitive Behavioral Therapy? APA. Retrieved November 2, 2022 from https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
[16] Hedman, E., Botella, C, & Berger, T. (2016) Internet-based cognitive behavior therapy for social anxiety disorder. In N. Lindefors & G. Andersson (Eds.), Guided internet-based treatments in psychiatry (pp. 53–78). Springer International Publishing. Retrieved November 2, 2022 from https://doi.org/10.1007/978-3-319-06083-5_4
[17] Cuppers et al., (2014). Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry Journal. 2014 Feb; 13(1): 56–67. Published online 2014 Feb 4 doi: 10.1002/wps.20089. Retrieved on November 2, 2022 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3918025/
[18] Psychology Today (n.d.). Humanistic Therapy. Psychology Today. Retrieved November 2, 2022 from https://www.psychologytoday.com/ca/therapy-types/humanistic-therapy
Navigating the Holidays When You’re in Recovery
Navigating the Holidays When You’re in Recovery

It’s the time of year where invitations to gather with family, friends and co-workers are plentiful. For some the memories and celebrations attached to the season can be big ‘triggers’. But don’t worry about your social calendar. Manage it!
Seasonal celebrations and holidays can be wonderful times for people to come together. Families, workplaces and community organizations often host events that can be fun to attend, but they can also be sources of stress for many people. For someone in recovery, however; these kinds of gatherings can be particularly challenging as they may involve a lot of triggers or tempting environments. You know you’ll be invited to attend, but what if you’re already feeling nervous about how to respond?
Under pressure
Realize that you are probably putting unnecessary pressure on yourself if you are thinking that you have to accept every invitation you get. The last thing you need is to be stressed about going to your aunt’s for dinner and then meeting up with your co-workers at a holiday bash. Sometimes there are simply too many things going on. It’s totally fine to pick some, or even none of them based on how you feel at this point in your recovery. Your number one responsibility is to your health and well-being. So, the main principle that should guide your social calendar is: what is healthiest for you, and what’s best for your sobriety!
It would be great if people treated addictions the way they treat allergies – with sensitivity, understanding and extra effort to make sure you’ll be safe. Small steps can lead to big changes. Take the first one by focusing on yourself. Start each day with a little promise to yourself you will do your best to stay sober.
Go ahead. Make plans…but not that kind
The next few steps you take are about acknowledging your feelings and addressing your anticipation. You need to spend time thinking about what could happen at these events and what is going to help you feel good and be confident so that you can keep your promise. Here are four strategies you can use to think this through:
1. Be honest with yourself
Take a few minutes to consider how you are feeling about your recovery at this point in time. What words come to mind? Are you feeling strong? Would you say you are vulnerable? Perhaps you’re excited? Or anxious? Or maybe you’re nervous? What are the strengths and tools that can aide you in your recovery, during this period?
Write all of these feelings and words down and then leave them for a few hours. Come back to them later in the day. Do you feel the same way? Thinking about your feelings and then releasing your thoughts can be a powerful way to help you be aware of where you are right now, in the present moment.
2. Be realistic about how these events can make you feel
Look at all of these occasions and instead of thinking about what’s in it for me, think about what could it do to me? Interacting with family, friends and co-workers can be exhausting and stressful, making you more susceptible to going along with whatever they are doing. You need to stay focused, fed and well rested, so your decision making is clear and confident. When you’re tired, hungry and distracted, it’s easier to be persuaded to abandon your plan.
3. Be kind to yourself. Guilt-free
Give yourself permission to bow out when you’re not sure how an event will go. Don’t ever feel pressured or obligated to show up to each and every occasion you might be invited to. Be kind enough to yourself to figure out what the purpose of the occasion is from your point of view. It’s all about perspective. If you are struggling with finding a meaning that feels right, then take a pass. Remember, send your regrets, but don’t think that you need to offer a lengthy explanation.
4. Be aware of your triggers and be ready to act
Knowing how you tend to react when you encounter one of your triggers helps you learn to avoid them. Face it: these could come up when you least expect them and be related to times of day, places, people or situations. Realize that these feelings and temptations are associations and also that they will pass. Cravings are just emotions that your brain is using to tell you how to behave [Heshmat 2015]. They usually only last about 20-30 minutes, and then they diminish. While they’re at their most intense during that time, you can redirect your thinking. Get a change of scenery and go for a walk, try finding a quiet place to meditate or focus on deep breathing, or call someone in your support network to talk.
All in the family
When you do decide to partake in a holiday gathering, there are some tips you can use to make hanging with the cousins more bearable. In all families, some people are supportive, and others are not. It’s important to be prepared for this during the holidays. Take inventory of who you know is tactful, trustworthy, and respectful. Spend time with them and avoid the unsupportive people as much as possible. You might even want to speak with the hosts beforehand and share your concerns. Talk about how you will — and how they should — respond if a situation arises. Talk about what you will be saying to decline offers you may get from other guests like: ‘Have a drink with me!’, ‘It’s only one!’ and ‘Come on, it’s a party, have some fun!’ and ask for their support. It doesn’t mean they need to make an announcement or “prepare people” before they arrive. It’s about being honest and building a better response to the situation. It helps to have a script of what you will say to people, to explain that you’re not going to be drinking. You can limit it to what you’re comfortable sharing, but it should include a clear, assertive “no” message, with no room for negotiation.
Above all, do your best to stay calm. Remember that there is no perfect family gathering. Things are always messy. If you feel like the situation is going to cause you pain, it may not be the right time for you to attend. And that’s okay. You don’t want to have feelings of added tension, stress or guilt associated with anyone or the holiday celebrations themselves.
Come on everybody: attending parties with friends and co-workers
Celebrating with friends and co-workers may be different from family gatherings, but these events can also cause you stress. Thankfully, you can use some of the same strategies you put in place to deal with that dinner. Stick with people you know and trust who support you. Avoid those you don’t know and watch out for those whose intentions you instinctively aren’t sure of. Stay calm in all interactions and do some party planning of your own beforehand.
Make party plans
1. Set goals and times for yourself
Arrive early and be prepared to leave early too if you find you’re having a difficult time being around people who are drinking. As parties go on longer, people tend to drink more and become more relaxed and take things in a different direction. Leaving before things get wilder isn’t a bad thing. You’ll be in control and not have any next-day regrets.
2. Consider bringing your own beverages (BYOB)
Sometimes you can bring your own drinks to be sure you have complete control of what you’re consuming. You won’t have to worry about anyone accidentally making a drink for you that is going to trigger a setback in your recovery.
3.Use the buddy system
Have someone who you trust and can rely on to recognize a situation that may be developing, distract you and intervene if something goes wrong. Your buddy should be completely sober: no drinking, smoking or using drugs. This person is going to act as your advocate.
4. Be the one who others lean on
Having responsibility for others can sometimes help reduce the stress you are feeling. Why not consider offering to be the designated driver for a group of people? It’s a role that everyone will understand is essential and not question your motivations or actions. As the driver, you’ll also be able to leave when you want to.
What to do if you experience a slip or lapse
Addiction and relapse are not only about the substances, but also about the emotional voids you are trying to fill. Relapse is often a part of the recovery journey, but the emotional responses it can incite can be devastating.
Don’t let yourself get stuck. And don’t be too hard on yourself. If you feel hopeless, humiliated or guilty, be open to finding hope again. Work through any anger or fear and find the courage to be honest and begin addressing the underlying issues that caused you to slip. When needed, be sure to seek social support from people you trust and seek professional help when you need it.
With determination and a little help, you can find your way again.
References
1. Heshmat, S. Ph.D. (January 7, 2015). Why Cravings Occur. Cravings and Trigger factors. Psychology Today.
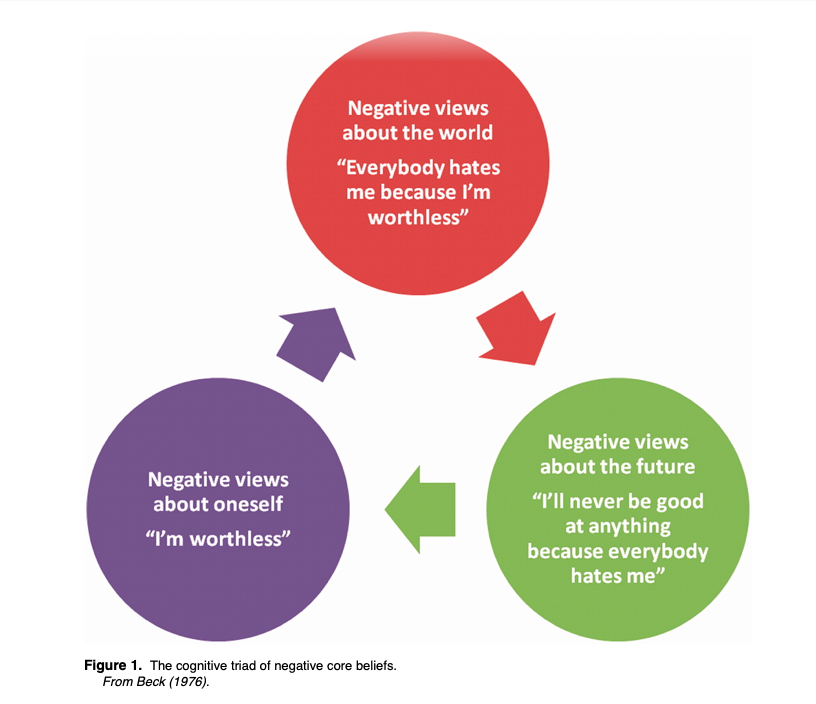 [6]
[6]