Navigating Panic Disorder: Understanding, Coping and Supporting
Navigating Panic Disorder: Understanding, Coping and Supporting

We regularly encounter stressful and challenging situations that can heighten our anxiety or fear. But sometimes, an experience can be particularly overwhelming, and our bodies react instinctively with a physical and emotional intensity that kickstarts our fight-or-flight response. Because of intrusive thoughts, it’s suddenly hard to breathe; we feel our heart racing or that we’re having chest pains and start sweating. Detached from our surroundings, while consumed by racing thoughts and a sense of impending doom, we feel like we’ve lost control. Panic attacks are highly distressing and disruptive.
When panic attacks begin to occur repeatedly, however, the person experiencing them might start to be consumed with worry about the potential and unpredictable nature of future episodes, so much so that the fear of that possibility begins to affect their behaviour and lifestyle significantly. This is known as panic disorder. In these situations, where a pattern of recurring panic attacks develops, it is essential to seek professional help.
In this article, we’ll look at the concept of a panic attack versus panic disorder. Not everyone who experiences a panic attack will have panic disorder, but those with panic disorder will often experience repeated panic attacks. Panic attacks can occur with any anxiety disorder as well as other mental disorders (e.g., PTSD, substance use disorders, depressive disorders) and some medical conditions (e.g., cardiac, gastrointestinal, respiratory, vestibular). We’ll explore the relationship with agoraphobia, discuss some treatment options and coping strategies that can help support someone with greater empathy and understanding. From there, we’ll also address how veterans can be at increased risk of developing panic disorder and share resources that are essential to creating a supportive environment and helping to destigmatize mental health concerns.
What is panic disorder?
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), panic disorder can be diagnosed when someone frequently experiences recurring and unexpected panic attacks and is persistently worried about having more panic attacks or changes their behaviour in maladaptive ways because of the panic attacks (e.g., avoidance of exercise or of unfamiliar locations). (1) Panic disorder is not the same as an anxiety or a panic attack, though both can be elements of this type of mental health condition.
| Anxiety | Panic Attack | Panic Disorder |
| Feeling uneasy | A sudden, intense surge of fear | Repeated, unexpected, and unpredictable panic attacks. |
| Constant worry about having future panic attacks can heighten anxiety. | ||
| Intense and overwhelming feeling of losing control.Persistent fear that something terrible will happen during a panic attack. | ||
| Example: You might feel anxious before taking a test or making an important decision. | Example: You might experience a panic attack if you are afraid of heights and go on a Ferris wheel. | Example: You might be experiencing panic disorder if, during a panic attack, you feel intense physical and emotional symptoms. Your pulse might start pounding so intensely that you begin to think you are having a heart attack. It could lead to waves of successive or simultaneous panic attacks where you start to feel short of breath and dizzy or begin to sweat and have abdominal pain. You may be unable to determine the cause of your panic attacks because no obvious danger could have triggered them. You will often start to worry about when the next attack will happen. There could be more today, this week, or this month. |
Panic disorder can make daily life challenging and can affect a person’s comfort with social interaction. They may prefer to stay within what they determine to be a safer environment where they are close to exits and have ways to escape a situation if a panic attack does happen. There may be a lot of pre-planning for outings, so they feel prepared by having medication or trusted friends and family members nearby. What someone with panic disorder is experiencing is real and should never be thought of as an overreaction.
It’s important to note that not everyone who has experienced anxiety or had a panic attack will go on to develop panic disorder. It’s estimated that:
-
- While up to 1/3 of Canadian adults may have a panic attack, about 4% of them will experience panic disorder in their lifetime (2)
-
-
- Up to 11% of people in the US experience a panic attack (3)
-
-
- Approximately 2-3% of them have panic disorder (4)
-
-
- Onset often occurs in the late teens and early twenties (5)
-
-
- It often affects women more than men (6)
Signs and Symptoms
Panic attacks can vary in their abrupt peak of intense fear or intense discomfort and peak in intensity within a few minutes. (7) People can experience physical symptoms like:
-
- Racing heart
- Shortness of breath
- Trembling
- Chest pain
- Dizziness
- Sweating
-
Emotionally, someone may feel intense fear, impending doom or like they have lost control. It’s important to note that for the person going through a panic attack, their perception of time can be distorted, making the experience feel much longer.
With panic disorder, frequency, intensity, and duration help determine different degrees and classifications of symptoms: (8)
| Type 1 | Type 2 | Type 3 | Type 4 |
| A single panic attack. | Frequent panic attacks (without depression). | Regular and recurring attacks with the gradual development of additional symptoms such as anticipatory anxiety, general anxiety, or agoraphobia. | Recurring panic attacks with additional symptoms, including depression. |
The Relationship with Agoraphobia
Agoraphobia is intense anxiety because of thoughts about being in situations or places where it can be difficult to leave or get help. The spaces are usually either open “such as parking lots, marketplaces, bridges) or enclosed, “such as tunnels, small rooms and elevators,” as well as “supermarkets, shopping malls and other crowded places,” including public transportation and unfamiliar environments. (9) People experiencing agoraphobia can feel trapped, helpless, or embarrassed as the worry that they may experience a panic attack overwhelms them. In some cases, someone experiencing panic disorder with agoraphobia “may not be able to leave the house.” (10) While symptoms of agoraphobia can exist without experiencing a panic attack, with panic disorder, there is no apparent reason for the agoraphobia to be present.
Veterans and Panic Disorder
Veterans can be at increased risk of developing panic disorder and substance use disorder due to the nature of their roles and exposure to combat, traumatic experiences and heightened general stress they experience during deployment. Programs like the Guardians Program, https://homewoodhealthcentre.com/treatment-programs/guardians-program/, at the Homewood Health Centre can offer specialized mental health support for veterans.
Treatment Options
There are a few treatment approaches that are effective to help with panic disorder. Working with a doctor is the best place to start, as they can help you understand what might work well and consider combinations that could provide relief more rapidly.
| Psychotherapy | Medication | Complementary and Alternative Therapies |
| Cognitive-Behavioural Therapy (CBT)Helps identify symptoms and triggers, plus develop ways to cope and change behaviours. Exposure Therapy Helps address associations between fears and bad outcomes to help manage anxious feelings. | Depending on which medications your doctor might recommend, relief can happen within a few weeks. Some medicines may take longer to see improvements. Your doctor will discuss possible side effects and work to find a medication that works. | Art therapy Breath training Both types of treatment can be helpful. Because they help reduce stress, plus develop calm and healthy mindfulness and self-regulation techniques when you practice them. Sometimes, these methods are easier for people to use to help them complete any ‘homework’ from psychotherapy treatment. |
Coping Strategies
Meditation and lifestyle choices such as prioritizing better sleep, regular exercise, a balanced diet and limiting alcohol intake, plus maintaining social connections, are always good ways to cope with life’s stressful situations. Some specific techniques can be helpful to try when experiencing anxiety or panic attacks:
- Breathing and relaxation techniques can help regulate the body’s stress response by introducing a rhythm that helps calm our automatic nervous system responses and reduce anxiety.
- The 555 breathing technique involves inhaling for a count of 5, holding the breath for a count of 5 and then exhaling for a count of 5.
- Box breathing is similar in that it involves inhaling for a specific count, holding the breath for the exact count, and exhaling for the same count. With box breathing, you add a counted pause before starting the cycle. Practitioners sometimes suggest envisioning a box shape to complete the technique.
- Mindfulness practices that help focus on sensory awareness and offer grounding can also help during a panic attack and promote overall well-being. These exercises can help shift attention away from anxious thoughts.
- The 333 sensory awareness technique involves identifying and acknowledging three things you can see, three things you can hear, and three things you can touch in your immediate surroundings.
- The 54321 technique is similar but includes even more sensory awareness. You focus on naming five things you can see, four things you can touch, three things you can hear, two things you can smell and one thing you can taste.
How to Support Someone During a Panic Attack
- Understand the nature of a panic attack and remember you are there to support someone experiencing one.
- Remain calm and provide reassurance, emphasizing that the panicked feelings will pass. Talk using short sentences.
- Encourage the person to use coping strategies that they may have learned in therapy or that you are aware of, like mindful breathing and grounding techniques. Even simply helping them count slowly aloud to ten can help slow their heart rate and make them more responsive.
-
-
-
Developing awareness and understanding of panic disorder is crucial to fostering compassion, being supportive and eliminating stigma around mental health. Knowing some signs and symptoms can help all of us create a better sense living in a supportive community.
References:
1. American Psychiatric Association. (2013). Anxiety disorders. Retrieved January 12, 2024 from Diagnostic and statistical manual of mental disorders (5th ed.).
2. Canadian Mental Health Association – British Columbia Division (n.d.). Panic Disorder. CMHC BC. Retrieved January 1, 2024 from https://bc.cmha.ca/documents/panic-disorder-2/
3. Cleveland Clinic (medically reviewed) (2023 Feb 12). Panic Attacks & Panic Disorder. Cleveland Clinic. Retrieved January 1, 2024 from https://my.clevelandclinic.org/health/diseases/445…
4. Ibid.
5. Burke D., and Collins D. (medically reviewed) (2022 Feb 23). A guide to Panic Attacks and Panic Disorder. healthline. Retrieved January 1, 2024 from https://www.healthline.com/health/panic-disorder
6. Ibid.
7. American Psychiatric Association. (2013). Anxiety disorders. Retrieved January 12, 2024 from Diagnostic and statistical manual of mental disorders (5th ed.).
8. Takeuchi, T. et al. (2022 March). Four clinical types of panic disorders – Abstract. National Library of Medicine. Retrieved January 1, 2024 from https://pubmed.ncbi.nlm.nih.gov/1635333/#:~:text=T…
9. Antony, M. Ph.D. (2002). Panic Disorder and Agoraphobia. St. Joseph’s Healthcare Hamilton. Retrieved January 1, 2024 from https://www.stjoes.ca/health-services/mental-healt…
10. Ibid.
The Role of Occupational Therapy in Mental Health Treatment
The Role of Occupational Therapy in Mental Health Treatment

In 2022, more than five million people in Canada met the diagnostic criteria for a mood, anxiety, or substance-use disorder, which amounts to about 13% of the population. For many, poor mental health is a barrier to living a full and productive life. Occupational therapy is a mental health treatment that can help them learn to adapt and participate more fully in the activities that give their lives stability, purpose, and joy.
Repairing connections to daily life 
Mental illness impacts every aspect of a person’s life, including their ability to participate fully in social, recreational, and employment activities. People who face mental health challenges can find themselves unable to work, attend school, or even enjoy activities such as hobbies or sports. As a result, their world becomes smaller and they become more isolated as their connections with the outside world are broken.
Among employed Canadians, 7.5% said they had taken time off from their job or business because of stress or for mental health reasons in the 12 months before April 2023. Every week, about 500,000 Canadians are unable to work due to poor mental health, resulting in 16% of working hours being lost to absences and presenteeism due to mental health issues.
Being unable to work has consequences that go beyond financial uncertainty. Work is a fundamental aspect of our identity and role within society. It gives structure to our lives, provides us with a sense of purpose and belonging, and brings us the respect of our peers.
The same is true of school, and similarly, the ability to attend school regularly is often interrupted by mental illness. A 2017 Ipsos survey of Ontario youth found that 46% of students surveyed reported missing school because of anxiety. And when they do attend, they don’t see as much benefit from the experience: children with poor mental health are 3.5 times likelier to have average grades of C or lower, and 25 times likelier to experience difficulty making friends.
Occupational therapy and mental health
Occupational therapy is used in many contexts, and occupational therapists can be found in a variety of settings. In a school, you may find them helping children develop skills and behaviours that will help them thrive in an academic setting. In a hospital, they can be found helping people with cognitive or physical limitations re-learn specific tasks or find new ways of doing things so that they can regain independence. In a mental health and addiction treatment centre, occupational therapists help people with depression, anxiety, post-traumatic stress disorder (PTSD), addiction, and co-occurring disorders to manage their conditions and regain their ability to take part in the everyday activities that make up daily life.
While physicians and psychiatrists make diagnoses, prescribe medication, and create individual treatment programs, occupational therapists help people with mental health conditions learn new ways of participating in work, school, and leisure activities by regaining or acquiring new skills, and adapting their environment (or their response to it) in ways that make it easier for them to participate in various activities.
 Part of an integrated mental health treatment
Part of an integrated mental health treatment
Mental health treatment requires a holistic approach that supports the whole person, including physical, mental, emotional, social, cultural, and spiritual components. Occupational therapists work closely with other practitioners and specialists to form a collaborative team that delivers holistic care.
This team can include physicians, psychiatrists, physiotherapists, prime therapists, nursing staff, addiction specialists, registered dieticians, recreational therapists, music therapists, art therapists, and horticultural therapists.
The role of the occupational therapist is unique in that it overlaps with and complements many other disciplines. In the context of mental health treatment, occupational therapy focuses on how the patient’s mental state—their thoughts and emotions as well as the symptoms of mental illness, such as fatigue, loss of motivation and meaning, fearfulness and hypervigilance—are preventing them from participating fully in every aspect of a balanced life.
How occupational therapy aids in mental health treatment
At Ravensview, a private mental health and addiction treatment centre on Vancouver Island, British Columbia, the occupational therapist uses a range of evidence-based approaches to support their patients in returning confidently to day-to-day life. These approaches can include:
Cognitive restructuring techniques: These therapeutic techniques help people recognize, challenge, and change negative thinking patterns that can become limiting and self-defeating.
Problem-solving skills training: This intervention gives patients the tools they need to identify problems and find ways to solve or adapt to them.
Activity exposure: Within an inpatient setting, occupational therapists help the patient build confidence by giving them a safe, controlled way to acclimatize to the environment and activity that they need or want to return to.
Supportive structure: Occupational therapists often help patients to create daily routines and set specific goals that help them progress along a path toward the desired lifestyle.
Motivational interviewing: Through empathetic, person-centred counselling, occupational therapists explore and resolve ambivalence, build personal motivation, and develop a plan for behavioural change.
During the treatment, the occupational therapist identifies medical and non-medical issues that are impacting the patient’s capacity, helps the patient improve their ability to identify and manage those issues, and supports the patient in strengthening their motivation for returning to work, school, or social and leisure activities.
The impact of occupational therapy
Effective mental health treatment takes a multidimensional view of a person’s life, including work, school, recreation, hobbies, and human interaction. By helping patients reconnect with these dimensions, occupational therapy can play a significant role in a patient’s recovery.
Including occupational therapy in a patient’s treatment journey can help to break a vicious cycle, where a person with mental illness withdraws from work, school, exercise, leisure, and social activities, which in turn puts them at greater risk of poor mental health. In fact, this type of therapy can help to accelerate recovery by creating a “flywheel” effect, where the return to fulfilling activities helps to accelerate the patient’s return to health through participation in meaningful and beneficial activities.
Occupational therapy helps people with mental health issues achieve a number of crucial recovery milestones:
Increase physical movement. The link between exercise and mental health has been extensively researched and confirmed. Evidence from a meta-analysis of 49 studies spanning 260,000 participants shows that people with higher physical activity levels are less likely to develop depression, which is why recreational therapy also plays an integral role in mental health treatment.
Get back to work. The inability to perform work has financial and psychological consequences, resulting in a loss of self-esteem, work relationships, structure, and purpose. A meta-analysis found that 14 of 16 longitudinal studies on the impact of unemployment and mental health showed a significant, negative association. By helping people return to gainful, meaningful employment, occupational therapy improves their mental health.
Create social connections. Depression, anxiety and cognitive decline (in older people) are all associated with social isolation and having fewer social ties. Research from Statistics Canada showed that 62% of socially connected people with mental health-related disabilities rated their mental health positively compared to only 49% of those who were not socially connected.
Enjoy hobbies. Research shows that having a hobby is linked to lower levels of depression – and may even prevent depression for some people—even those who have clinical depression. Spending time outside in nature has also been shown to have a protective effect on mental health, as do creative pastimes such as music and art.
We are what we do
For most of us, what we do on a daily basis defines us and gives us our sense of identity and self-worth, whether it’s the contribution we make to the world through our work or the things we do in our down-time that bring us joy. When we experience a mental illness, we often lose those essential parts of ourselves. Occupational therapists help patients find ways of regaining them so that they can participate in and benefit from a return to normal, daily life.
Trauma Informed Collaboration
Trauma Informed Collaboration

We refer to the strong emotions that can unexpectedly affect our ability to maintain our steady state as trauma. Researchers continue to learn how our bodies can hold onto the memories of these traumatic events, even those that may have occurred very early in our childhood. Unfortunately, “few people go through life without encountering some kind of trauma” through no fault of their own. (1)
However, we can change how we interact with others to be more trauma informed. When we are willing to develop an awareness that the prevalence of trauma is significant and decide to operate with that knowledge and consideration, we can find more success in our interactions and collaborations with others.
This article will explore some of the fundamentals of trauma informed collaboration as a respectful, supportive approach that helps build resilience.
What is trauma?
Many people “mistake ordinary hardship or distress for genuine trauma”, which can lead to them start using the word, trauma, as they reflect on various life incidents and memories.(2) Not every difficult situation is categorically traumatic, and not all traumatic events will be debilitating. Most of the time, we can move beyond the initial feelings that these bad experiences stir in us. When these experiences don’t easily fade into memory, they could be viewed as causing longer-term harm.
For something to be classified as traumatic in the psychological sense of the definition, the experience is:
- Out of the person’s control
- Sudden and unexpected
- Harmful or life-threatening
- Damaging to a person’s sense of safety
- Responsible for creating overwhelming vulnerability (3)
Trauma affects the body’s sympathetic nervous system by creating a state where it perceives it is constantly at risk and should be ready to respond to threats at any moment. Living with this kind of hypervigilance means that the body’s usual fight, flight and freeze responses are always activated. The stress hormones and adrenaline our bodies produce continue to circulate rather than follow the expected path of clearing out of our systems when the crisis ends so that we can return to a more relaxed state.
Researchers like Dr. Bessel van der Kolk and Dr. Gabor Maté, who have studied and helped to classify the many different types of trauma, have shown that over time, unresolved or even unconscious trauma disturbs both physical and emotional functions. These disruptions can cause everything from pain and sleeping problems, to chronic illness and severe emotional disturbances that affect someone’s sense of who they are and their relationships.
It may be helpful to realize that trauma can: (4)
- Affect as a single event or repeated occurrences of events over time
- Arise from interpersonal relationships of people who know each other
- Influence developmental stages and patterns of emotional, social, and psychological growth
- Be political in nature, threatening people’s lives, beliefs, culture, and livelihoods
What is trauma informed collaboration?
Trauma informed collaboration is an approach you can adopt as a regular part of how you interact with people daily. It means that you acknowledge and are aware of and have an appreciation that inputs – even of the most seemingly innocuous nature – can create sensory overloads in people that are traumatic responses. When someone reacts unexpectedly, it can be challenging to understand why. Sometimes it can turn a situation into one that is unintentionally counterproductive and can damage our relationships and, potentially, even future interactions. By becoming trauma informed, we can influence the outcomes of our interactions so they have the potential to be more consistent, positive, and productive for everyone.
Is this what it means when we hear something is triggering for someone?
A trigger is an association someone makes that can inadvertently kick-off “re-traumatizing interactions” that cause them to experience a “dysregulated” or intense stress response. (5) Being triggered means someone is re-experiencing trauma. It isn’t just being “uncomfortable “or sensitive or feeling that something is “rubbing you the wrong way.” (6) A person may only be aware that something will necessarily act as a trigger for them once it happens.
Being more trauma informed, that is, aware of how far-reaching trauma can be, means that we can become more attuned to signals in people’s body language that indicate someone is displaying a traumatic stress reaction.
Here’s what you might notice: (7)
- A shift in someone’s posture where they appear more nervous, uneasy, or afraid by shifting their position frequently, withdrawing or even turning their body away from an interaction.
- Trembling fingers, clenching and unclenching of fists, fidgeting, or using something physical that is nearby to create a protective barrier (such as a bag, pillow or book).
- Self-soothing gestures such as putting a hand on their head, neck, or lap.
- Rapid and quick facial expressions such as
- oraised, lowered, or furrowed eyebrows
- ofrowning or lowering of lip corners, pursed lips, or lip biting.
- Reluctance to make eye contact, looking bored, off to the side, or off in the distance.
- Crossed arms and legs, tapping and jiggling feet.
- A higher-pitched tone of voice, more rapid speech than usual, or speaking slowly and quietly or with definitive emphasis on certain words.
Why is trauma informed collaboration important?
Operating with the knowledge that most people have experienced traumatic events is a supportive approach that actively demonstrates that you are caring and compassionate about your connections and relationships with others in your own life. It also is a way to influence interactions, experiences, and environments to make them healthier at home, in the community, or at work. You might help someone who is having trouble regulating their emotions or reduce the chance that they could display challenging behaviours.
Developing your trauma informed approach takes time. As you learn, conscious practice will help you to build better relationships. More and more healthcare professionals are adopting this approach as a standard of care because they realize the benefits. You may have heard it referred to as person-centred care. (8)
How does the prevalence of trauma affect people’s experiences of seemingly ordinary events?
It may be surprising to learn how significantly trauma affects nearly everyone.
- 70% of U.S. adults have experienced some traumatic event at least once in their lives (9)
- 75% of Canadians will experience at least one traumatic event in their lifetime (10)
- 1 in 10 people in Canada have been diagnosed with PTSD (11)
Often, people display symptoms of trauma in their interactions with others. These can present as: (12)
- Physical changes
- Headaches, heart rate increase, sweating
- Exhaustion, loss of appetite, loss of libido
- More susceptible to illness
- Constipation/diarrhea
- Hypersensitivity or hyperawareness (to sounds and/or touch)
- Harmful indulgences (alcohol, drugs, food)
- Emotional changes
- Fear, depression, anxiety, panic
- Extreme mood swings, rage, anger
- Withdrawal or isolation
- Guilt, blame, shame
- Loss of interest in regular activities
- Flashbacks or nightmares (PTSD)
- All of these emotional changes could stem from a PTSD diagnosis,however, some or few people go on to develop what we consider PTSD (13)
Why is it essential to adopt a trauma informed collaborative approach?
This approach aids our ability to respond to stressful situations in healthy ways. It might help to think about it using these five words: (14)
- Realize that stress and trauma happen to all of us.
- Recognize that our reactions are attempts to feel safe again.
- Respond with understanding, compassion, and patience every time.
- Resist re-traumatizing to boost emotional safety and avoid triggering events proactively.
- Resilience helps keep the focus on people’s strengths.
By adopting principles founded in safety, empowerment, trust, transparency, collaboration, supportive help, and attentiveness to historical and cultural issues, you’ll become more confident in yourself and those you are interacting with. Think about how this approach could be beneficial for equity deserving groups, such as the LGBTQ2S+ community, and actively work to address misogyny, racism, and marginalization.
Trauma informed collaboration helps you develop healthy and appropriate boundaries. It allows you to intentionally lead from a place of empathy in all your interactions. It’s a powerful tool that can alleviate or eliminate discrimination, promote understanding, and support harmony in co-existing despite our differences.
References:
1. Psychology Today Staff (n.d.). Trauma. Psychology Today. Retrieved, May 19, 2023 from https://www.psychologytoday.com/ca/basics/trauma
2. Ibid.
3. Ibid.
4. Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
5. Dubé, Kate, LCSW. (2021 July 22) Trauma Informed Care: What is it and Why is it Important? FOOTHOLD Technology: Mental Health. Retrieved May 19, 2023 from https://footholdtechnology.com/news/trauma-informe…
6. Cuncic, Arlin. (updated 2022 March 10). What Does It Mean to Be ‘Triggered’ – Types of Triggering Events and Coping Strategies. Very Well Mind.com. Retrieved May 19, 2023 from https://www.verywellmind.com/what-does-it-mean-to-…
7. Good Therapy (updated 2019 November 1). What Is Your Client’s Body Language Telling You? ˆ Good Therapy.org. Retrieved May 19, 2023 from https://www.goodtherapy.org/for-professionals/mark…
8. Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
9. The National Council for Behavioral Health (n.d.). How to Manage Trauma. The National Council.org. Retrieved May 19, 2023 from https://www.thenationalcouncil.org/wp-content/uplo…
10.Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
11. Ibid.
12. The National Council for Behavioral Health (n.d.). How to Manage Trauma. The National Council.org. Retrieved May 19, 2023 from https://www.thenationalcouncil.org/wp-content/uplo…
13. Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
14. Ibid.
Celebrating Pride Means Supporting 2SLGBTQ+ Mental Health
Celebrating Pride Means Supporting 2SLGBTQ+ Mental Health

June is a time for celebrating the diversity of Canada’s 2SLGBTQ+ communities. But it’s also a time to reflect on how we can nurture and support that diversity every day of the year.
The 2SLGBTQ+ community is disproportionately affected by mental health and addiction issues, and it prevents many of its members from living their best lives and reaching their full potential. For families, friends, and caregivers alike, changing the way we think about 2SLGBTQ mental health and addiction treatment and recovery can transform the outcomes.
Progress and challenges
There is much to celebrate during this year’s Pride Month. As of 2023, Canada is home to one million individuals who identify as 2SLGBTQ+, which represents 4% of the total population aged 15 and older. Three-quarters of Canadians support same-sex marriage, and 61% say they support LGBT people being open about their sexual orientation and gender identity with everyone. Just last year, the federal government unveiled a five-year, $100 million plan to support 2SLGBTQ+ communities across the country.
Yet in some ways, 2SLGBTQ+ visibility and acceptance have never felt more fragile as there is often backlash. Between 2019 and 2021, hate crimes based on sexual orientation rose nearly 60% to reach their highest level in five years.
More than ever, we need to make an effort to understand, celebrate, and make room for queer lives and identities, and that’s especially true when it comes to supporting 2SLGBTQ+ mental health and addiction treatment.
 The cost of being queer
The cost of being queer
In a perfect world, people of all genders and sexual orientations would be given equal opportunities to thrive. But the reality is that 2SLGBTQ+ Canadians still face multiple barriers to health, wealth, and wellbeing.
Many 2SLGBTQ+ Canadians live with the trauma caused by secrecy, stigma, discrimination, and fear. In addition to being the target of hate crimes, they are also more likely to experience financial distress, homelessness, and housing insecurity than heterosexual Canadians. Canadians who are 2SLGBTQ+ also have fewer job opportunities and earn significantly less than straight, male counterparts and experience frequent microaggressions at work. A lack of access to medical care, suboptimal healthcare experiences, and poorer health outcomes also diminish quality of life for queer people.
A mental health crisis
In the face of so many challenges, it’s unsurprising that the queer community sees a higher proportion of mental health and addiction issues.
Courtney Sullivan, Addiction and Mental Health Therapist and Support Coordinator at Homewood Health Centre, which is located in Guelph, Ontario and one of the largest mental health and addiction facilities in Canada, provides both outpatient and inpatient treatment for addiction and mental health. They work with clients who identify as queer, including individuals who may be experiencing homelessness, job loss, trauma, addiction, and a range of mental health issues.
“There is a lot of stigma towards the queer community,” they explained. “A lot of people have their families disown them or kick them out or withhold family support. A lot of queer youth, in particular, end up in the shelter system, which exposes them to trauma and substance use, and their mental health can get a lot more complex.”
Research shows that 2SLGBTQIA+ Canadians are seven times more likely to abuse drugs or other substances and five times more likely to have mental health issues. Sexual-minority Canadians are also approximately 25% more likely to contemplate suicide (40% vs. 15% for the general population) or have a mood or anxiety disorder (41% vs. 16%).
Treatment challenges
Not only do 2SLGBTQ+ have a higher likelihood of developing mental health issues and addictions, but their treatment journey is complicated by systemic ignorance and discrimination in the healthcare system.
According to a 2019 survey, 59% of nonbinary people were misgendered daily and only 47% felt comfortable discussing non-binary health concerns with their primary care provider. One in three said their primary healthcare provider had no knowledge about trans/non-binary health needs, and one in four did not have access to in-person spaces specific for non-binary people.
“There’s a large amount of queer people who don’t actually disclose their queerness to their health care providers,” said Sullivan. “The medical system doesn’t have the greatest history,” they continued, pointing out that as recently as the 1970s, homosexuality was classified as a mental disorder.
“People who do disclose to their doctors are often put in a position where they have to educate them about how healthcare should be delivered, which puts a huge burden on the queer community.”
It’s even more complicated for people with an intersectional identity that combines queerness with another identity that puts them at a systemic disadvantage, such as being a person of colour or an Indigenous person.
“Recovery programs and agencies and organizations really need to show their support to the queer community and signal that they are seen, that their experiences are respected, and that the facility is open to work with you,” Sullivan said.
While Sullivan advocates for big changes in the healthcare system, including hiring for diversity and developing organization-wide policies that reflect diverse perspectives, they also believe that small things can make a big difference. As an example, they described a recent situation when they brought a suicidal trans client who didn’t feel healthy at home to the hospital. Asking for help took tremendous courage, but the client was deadnamed three times in a row during the intake process, which almost made them reject treatment. (Deadnaming occurs when someone calls a transgender or non-binary person by the name they used before they transitioned. While deadnaming may be unintentional, it can feel stressful and traumatic because it questions or invalidates a person’s gender identity.)
“The hospital is supposed to be a healthy space, and most healthcare workers are well-intentioned, but systemic homophobia and racism can come out through the policies and the way things work,” they said. “Something as simple as restructuring medical charts so that gender information and preferred pronouns are easily available at a glance can change the experience. Or have care providers identify their pronouns, which is kind of like offering an invitation for that person to give you theirs too.”
S upporting 2SLGBTQ+ mental health
upporting 2SLGBTQ+ mental health
If you are a friend, partner, or family member of a 2SLGBTQ+ person exploring treatment options or actively in treatment or recovery, you can play an integral role in supporting their mental health and resilience.
For Sullivan, these communication tips can help to ensure they feel heard, seen, and supported throughout the journey.
Let them lead. “Your loved one might have a substance use issue, but if they’re not ready to hear it, don’t force it on them,” said Sullivan. “When people get scared, they make threats, like, ‘You need to get sober or else!’ But that ruins the opportunity and the trust.” Instead, let that person decide what they need and set the pace for treatment and recovery.
Keep an open mind. “Come at things with empathy and compassion. Listen to that person. Try to understand why they’re making the choices that they do.” Sullivan pointed out that for some members of the 2SLGBTQ+ community, the use of stimulants is an important part of their lifestyle and sexuality. “It all comes back down to the impact that the person’s substance use has on their life, and what that person identifies as being problematic.”
Respect their experience. “The trauma and the experiences that queer people have are different,” Sullivan explained. “Even if you’re cisgender and you get kicked out of your home, it’s still a different experience than someone being kicked out of their house because of who they are.” Respecting those differences can go a long way toward creating a space for authenticity and healing.
 Pride in mental health
Pride in mental health
Pride Month is a time to celebrate the queer community and bring attention to the challenges it continues to face. The elevated risk of mental health and addiction issues is an important part of the story, and one that Homewood Health Centre and other mental health and addiction facilities in Canada are highlighting this year. We all have a role to play in supporting and protecting the mental health of 2SLGBTQ+ individuals, and that role goes beyond raising the rainbow flag.
“We’re having a flag-raising ceremony in honour of Pride here at Homewood, but that’s just the first step,” said Sullivan. “It’s about creating intersectional representation. You want people of colour working in your organization, you want Indigenous perspectives, you want queer perspectives. Be willing to hear the experiences of the people you employ and the people you support. Find out what it is that they’re looking for.”
Learn more about LGBTQ+ mental health.
Learn how to support children who identify as LGBTQ2+.
3 Ways Families can Support People in Addiction Recovery
3 Ways Families can Support People in Addiction Recovery

“While most of us have experienced some pain and anguish in our family, that family system can be a source of strength in healing from that pain.”
Dr. Julie Burbidge
Clinical Director, Homewood Ravensview
The negative impacts of addiction on families is well known. Less well known is the positive impact families can have on the addiction recovery journey. Parents, grandparents, spouses, siblings, and even children can play a powerful role in supporting a family member in addiction recovery and beyond.
In this blog post, we look at the difference families can make in the recovery journey and what they can do to support their loved ones as they transition from an inpatient treatment program to daily life.
Family support has a measurable impact
Supportive family dynamics can have a transformative impact. Family support can uplift every aspect of an individual’s life, from emotional wellbeing to physical health to academic and career success.
Even for an issue as complex and uncompromising as addiction, family support can make a measurable difference.
- A study of nearly 1,200 women who underwent inpatient treatment for substance abuse found that those with supportive families were less likely to relapse within six months of their discharge.
- A study of adolescents undergoing substance use treatment found that those who perceived their parents to be highly supportive had better outcomes than those who did not.
- A meta-analysis of 16 research studies found addiction treatments that involve family are associated with a 6% reduction in substance use compared to individual therapies.
- 65% of Canadians in treatment for an addiction said marital, family, or other relationships were the most important factor in initiating recovery.
Supporting a family member on the path to sobriety is no easy task, but the research is clear: family support can make a big difference.
“Positive attitudes and reinforcement from family members can inspire clients’ commitment to recovery,” explained Dr. Julie Burbidge, the Clinical Director at Homewood Ravensview, a private inpatient facility for mental health and addiction recovery in British Columbia. “It can also help them adapt to new challenges or limitations as they reintegrate with the wider world after spending time in treatment.”
Discharge is not the destination
When an individual completes a treatment program, it’s a major milestone and a cause for celebration, but it’s not the end of the road.
After the individual is discharged, the journey continues as they learn to resume their daily lives while remaining sober. The transition can be overwhelming, and it’s a time when family support in addiction recovery may be most needed.
While this transitional period is critical, it can be overlooked and under-resourced, which is why Homewood Clinics developed a series of post-discharge supports for patients and their families. Individuals who complete treatment are invited to participate in 12-month virtual support groups that meet weekly to focus on recovery management. For their families, an optional virtual meeting with a clinician is held each month at Homewood Ravensview. The facility is also launching a self-serve video hub where over 70 minutes of educational content covers a range of topics including talking to children about treatment, setting healthy boundaries, and understanding the stages of change in the journey to recovery. This will replace the virtual monthly meetings, and is meant to allow for more flexibility on when and how families receive these resources.
“Transitions are difficult because they involve uncertainty,” said Dr. Burbidge. “The more time and effort you put into planning for and discussing the transition plan, the more effective it will be.”
How to show your support
Supporting the recovery of an individual with an addiction isn’t easy, even for experts with years of specialized experience and training. For family members who don’t have that advantage, it’s even more intimidating.
Emotional dimensions can create further challenges. Even in families unaffected by addiction, relationships can be complicated. When addiction and mental health issues are added to the mix, the dynamics can be even more volatile.
“Being prepared for the transition home of a family member involves understanding your role in the recovery process,” said Dr. Burbidge. “It also means accepting that family life after treatment will be different and making a commitment to rebuilding relationships.”
Educating yourself ahead of time can help you prepare to provide family support in addiction recovery. Here are three of the most beneficial strategies for showing up in meaningful and constructive ways.
Understand the dynamics of change
People who undergo treatment for addiction are asked to change in profound ways, and that cycle of change doesn’t stop when they are discharged.
“Sometimes family members have the misperception that their loved one will be ‘fixed’ or ‘healed’ when they leave treatment,” Dr. Burbidge explained. “Treatment is an important step in a person’s healing and recovery, but the process continues long after their discharge.”
Understanding the stages of change can help family members recognize, accept, and meet people where they are in the journey.
The most important thing to understand about the path to change is that it isn’t tidy and linear. Just as a person with diabetes or asthma can relapse after being released from treatment, a person in addiction recovery may experience a relapse as they work toward sustained change. A relapse shouldn’t be seen as a failure but as one stage among many in the recovery process.
Stages of Change
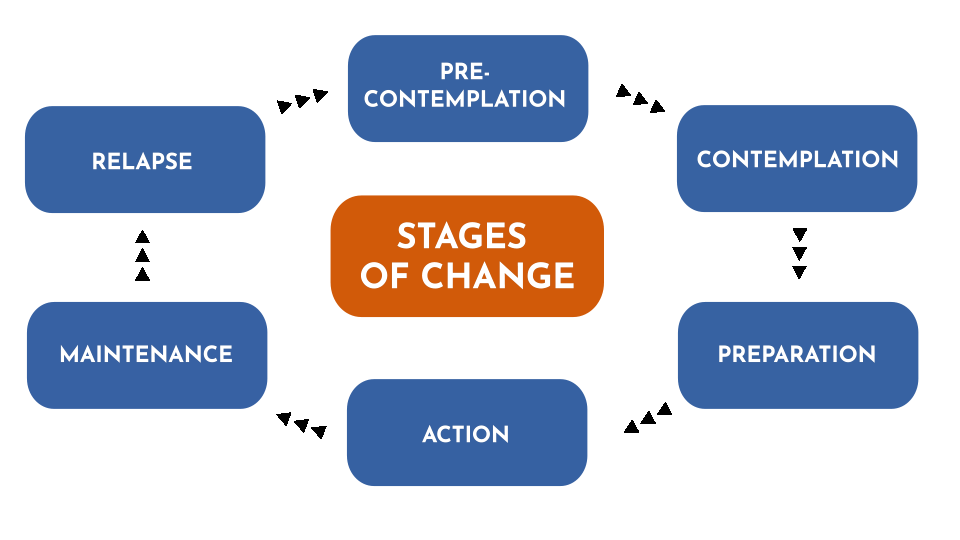
As people pursue their recovery, they cycle through various stages that can involve new thoughts, attitudes, and behaviours. Every journey is different, and few journeys are perfectly linear. This diagram represents the change model used by Homewood Ravensview, a private inpatient facility for mental health and addiction recovery in British Columbia.
There are several ways you can help to prevent or mitigate the impact of a relapse:
- Talk to the person in recovery about relapse so they know you understand it’s something that might happen.
- Let them know that you are there to support them and ask if they would like you to play a role in their relapse prevention plan.
- Pay attention to your own behaviours. Families can sometimes fall back into old, destructive patterns.
Learn to communicate effectively
Effective communication is the key to healthy interpersonal relationships, but it’s easy to slide into defensiveness and blame during times of stress and anxiety.
Dr. Burbidge advises family members to try using a form of assertive communication called “‘I’ statements” to create a connection with the person they’re speaking to and avoid slipping into harmful communication patterns that rely on accusing, blaming, and shaming. ‘I’ statements focus on your own experience and how you feel about it rather than focusing on what you think the other person is doing wrong.
“This gives us a way to express our feelings in a manner that is respectful and increases the likelihood that the other person will be open to hearing what we have to say,” said Dr. Burbidge.
You can express yourself with ‘I’ statements using a simple formula: “I feel [describe your feeling] when you [describe the person’s actions] because [describe the reason it makes you feel a certain way].
Here’s an example:
| Conventional ‘you’ statement | ‘I’ statement |
|
“You never listen to me. You make me so angry because you just don’t care enough about me to bother to listen when I’m trying to talk.”
|
“I feel angry when you interrupt me because It’s important to me that I’m able to share my ideas with you and feel heard by you.”
|
Set and respect boundaries
During treatment for addiction, people learn how to create boundaries as a way of staying on the path toward healing. As the family member of a person in recovery, you can support them by recognizing and respecting those boundaries. Setting boundaries of your own can also be very helpful in allowing you to preserve your energies and self-respect as you explore new ways of relating to that person.
“Boundaries are a way to establish where you end and other people or external influences begin,” explained Dr. Burbidge. “They are a way of setting healthy limits around what we will and won’t accept or do in our relationships with others.”
To set a healthy boundary with someone:
- Describe the boundary you are setting or the action that is causing you discomfort.
- Express how the situation makes you feel using ‘I’ statements.
- Describe the behavioural change you are looking for in the future.
- Without making threats, describe the action you will take if your boundary is crossed.
Here is an example:
“I feel angry when you interrupt me because It’s important to me that I’m able to share my ideas with you and feel heard by you. Moving forward, I would like it if we could each take turns speaking. This will help us better understand each other and hopefully feel more connected. The next time you interrupt me, I will leave the room and we can continue the conversation later.”
Take the next step together
An individual who has completed an inpatient addiction treatment program has done some hard and courageous work toward furthering their recovery. Re-entering their normal lives post-treatment is the next big step in their journey. By understanding the stages of that journey and learning new ways of communicating and interacting along the way, families can make a positive difference in the individual’s recovery experience and outcomes.
“To truly understand the individual, we have to understand the family system of that individual,” Dr. Burbidge said. “While most of us have experienced some pain and anguish in our family, that family system can be a source of strength in healing from that pain.”
For more insight into supporting a family member in addiction recovery, read these articles from Homewood Ravensview, an addiction treatment program in British Columbia, Canada.
Understanding Family Dynamics: What healthy family traits look like, and how to identify toxic family dynamics.
Supporting Those with Addiction: How to support family members who haven’t reached out for help yet.
Top 5 Tips to Motivate Someone with an Addiction, Towards Treatment
Top 5 Tips to Motivate Someone with an Addiction, Towards Treatment

1. Empathize, don’t criticize. Every time you point a finger, you could be pushing your loved one farther away. Ask questions and listen.There is great power in a supportive loved one communicating with empathy and without judgement.
2. Be firm but fair. Specify some ground rules. Make it clear to them that you will not support their addictive behaviour, and try to set healthy boundaries. With these boundaries in place, they may just be motivated enough to start thinking about quitting.
3. Tell them how you feel. Sometimes, a person living with addiction may not realize how their behaviour has affected you and others in their life. Don’t be afraid to share your feelings with them; doing so could show a significant level of care and support.
4. Use “I” statements. As you express your emotions to your loved one, make sure not to point fingers or fault toward them. They already suffer from their own guilt and shame, so you may risk them shutting down completely. Rather than passing blame and telling them what they did, turn it back around to you. Making statements using “I feel” instead of “you” can help promote healthy communication.
5. Address their fears. A huge factor in resisting treatment is fear of the unknown. Hop onto our site and educate yourself. Knowledge is power when it’s time to have that conversation.
How Stigma Impacts Post-Traumatic Stress Treatment for First Responders
How Stigma Impacts Post-Traumatic Stress Treatment for First Responders

You’re the one who answers the call.
The one who shows up.
The one who offers light through life’s darkest moments.
So how could you possibly be the one feeling lost?
Feeling lost is common for First Responders, even while at work doing what they love.
If you’ve experienced feeling lost, at work or at home, you’re certainly not alone.
First Responders and Post-traumatic Stress
The Canadian Mental Health Association (CMHA) says First Responders (police, firefighters, and paramedics), military personnel, doctors, and nurses all experience higher rates of post-traumatic stress than people in other professions.
For example, twice as many First Responders compared to the average population experience a post-traumatic stress injury. That’s according to The Center for Suicide Prevention.
Dr. Jonathan Wan, MD, FRCP(C), Medical Director at Homewood Ravensview adds that this can look quite different from person to person.
General signs of post-traumatic stress, according to Dr. Wan and the CMHA, include:
- Anxiety, avoidance, and dread about attending work
- Insomnia and/or nightmares about traumatic events
- Feeling “on edge” and full of physical tension
- Apathy or having reduced interest or pleasure in spending time with others or engaging in usually enjoyable activities
- Persistent self-blame or guilt related to traumatic experiences
- Re-experiencing the traumatic event
- Feeling detached from reality or lost, disengaged, not really present
- Emotional numbness or having hard time feeling or expressing emotions
- Concentration issues (ie., brain fog)
Stigma Still Exists. You Can Fight Back.
“Unfortunately, stigma for First Responders reaching out still exists today,” says Steve Farina, City of Coquitlam Fire Captain, Vice President of Lower Mainland North at BC Professional Fire Fighters Association and Vice-Chair of the BCPFFA’s Mental Health Taskforce and Occupational Health & Safety Committee.
Stigma can be internal (ie., self-stigma) or external (ie., from peers or institutions).
Internal stigma
“The biggest barrier for reaching out seems to be self-stigma (that internal conversation where one feels weak, fearful of being judged, etc.),” says Farina.
Dr. Wan further explains that despite greater awareness related to mental health issues, reaching out can still remain difficult.
“Part of the reason is because internalized stigma can present as the negative attitudes and self-judgement we have about our own experiences,” he says.
External stigma
External stigma can come from comments said by colleagues and supervisors, or fears about what they may say or think.
Negative perceptions (ie., judgements) and harmful behaviours such as gossip towards First Responders who have experienced mental health challenges or mental health conditions are examples of external stigma, says Farina.
Dr. Wan adds that external pressures can range from peers looking unfavorably on taking time away for recovery to institutions not acknowledging the impacts of psychological injuries.
“Whatever the source, stigma can compound mental health difficulties and prevent individuals who would benefit from treatment in seeking prompt care,” he says.
Expert Advice for First Responders
Farina says his advice for any new First Responder beginning their career is to connect to a mental health professional right away.
While we understand it’s not always easy to reach out, Farina suggests there’s benefit to seeking support sooner than later.
For First Responders with post-traumatic stress injury diagnoses, the accumulation of psychological injuries in the workplace at the expense of one’s health seems to be a common occurrence, he explains.
It’s vital for First Responders to understand their health and act accordingly, adds Wan.
“The saying of putting your own oxygen mask on in a plane before helping others is a fitting analogy,” says Dr. Wan.
“Don’t wait until your backpack is full of traumatic calls and stress and you’re overwhelmed, burned out, etc.,” he says.
Farina’s suggestions:
- Find a mental health professional you can trust and relate to
- Establish a relationship and baseline history early in your career
- Check-in regularly throughout your career
Leaving symptoms of post-traumatic stress untreated can build up into a traumatic stress injury or diagnosis of PTSD.
“PTSD usually appears within three months of a traumatic event, but sometimes symptoms may not appear for years,” according to the Canadian Mental Health Association.
The benefits of working with someone at any time, according to Farina, include learning tools to:
- Destress
- Down-regulate your nervous system
- Develop the awareness to know when to take a knee and reach out for help or additional support
If you’re already experiencing early signs and symptoms of post-traumatic stress, Farina encourages you to reach out and tell your supervisor, spouse, trusted coworker, or friend.
The Homewood Ravensview Difference
Come home to yourself at Homewood Ravensview.
Since opening in 2019, we’ve helped over 400 First Responders find their path forward from post-traumatic stress injuries.
We’ve made it part of our mission to continue learning and developing programming specific to the unique needs of this critical group. We do this by learning from people who get it because they have experienced something similar and know that while every trauma experience is different, you can heal from this injury, too.
Continual Learning
In partnership with Wounded Warriors Canada, Homewood Ravensview employees were given access to specialized occupational awareness training for the treatment of trauma-exposed professionals such as members of the Canadian Armed Forces (CAF), veterans, and other First Responders (ie., police, fire, emergency service professionals, etc).
The Introduction to Trauma-Exposed Professionals training program, developed by Wounded Warriors Canada’s co-National Clinical Advisor, Dr. Tim Black, has been designed to help increase competencies in the divide that exists between trauma-exposed professionals and the public.
The training program provides culturally-specific clinical approaches to support the complex mental health needs of trauma-exposed professionals and, through our partnership, is available to all Homewood Health employees.
Healing Outside of the Uniform: Guardians Program
The Guardians program at Ravensview supports First Responders in their journey in recovery from mental health difficulties.
Highlights of Treatment
- Personalized for your unique needs
- Medication consultation and management
- Access to group and individual therapy
- Ongoing assistance from trained professionals
- Peer support from other First Responders
Treatment starts with a comprehensive and multi-disciplinary assessment to better clarify your individual needs.
You’ll gain access to individual and group talk therapy and educational tools about psychology to support your overall wellness needs.
A diverse team of physicians will then discuss ongoing interventions that can include, but are certainly not limited to, medication management.
You’ll be involved in the process of your own medical care and get the support you, too, deserve.
According to Dr. Wan, every type of treatment occurs in a therapeutic setting with other First Responders. We’ve found this promotes safety and acceptance.
Homewood Ravensview believes in the transformative power of care because we’ve seen it firsthand. If you or someone you love feels lost from trauma or PTSD, take the first step – reach out. The courage to do so could be the beginning of your path forward.
Resources
- Canadian Mental Health Association. Post-traumatic Stress Disorder.
- Steve Farina, City of Coquitlam Fire Captain, Vice President of Lower Mainland North at BC Professional Fire Fighters Association and vice-chair of the BCPFFA’s Mental Health Taskforce and Occupational Health & Safety Committee.
- Dr. Jonathan Wan, MD, FRCP(C), Medical Director at Homewood Ravensview.
- The Center for Suicide Prevention. First Responders, Trauma & Suicide.
- BC First Responders Mental Health
June is National Post-Traumatic Stress Disorder Month
June is National Post-Traumatic Stress Disorder Month
PTSD does not discriminate; it can affect anyone regardless of their age, gender, or race.

Recent statistics from the Ministry of Veterans Affairs indicate PTSD as the second leading mental health disorder within the Canadian Armed Forces, with incident rates doubling between 2002 and 2013. However, PTSD is not limited to our military and soldiers. It can affect anyone who has experienced or witnessed a traumatic event.
Trauma is the Greek word for “wound”. While the Greeks used the term for physical injuries, trauma can also mean emotional and psychological wounds.
Trauma can refer to the traumatic event and the subsequent emotional and psychological injury. PTSD refers to a set of symptoms, which can be diagnosed as the condition of PTSD when the after effects of the trauma don’t go away within a specific time period.
What is PTSD?
Post-traumatic stress disorder (PTSD) is the psychological reaction to emotional trauma. This could include responses to powerful one-time incidents or chronic/repetitive experiences.
Examples of One Time Experiences:
Accidents, natural disasters, crimes, surgeries, death, other violent events
Examples of Chronic/Repetitive Experiences:
Child abuse, neglect, military combat, urban or domestic violence
Who is at risk?
PTSD does not discriminate; it can affect anyone regardless of their age, gender or race. PTSD is brought on by experiencing or witnessing a traumatic, often life-threatening event. At particular risk are individuals who work in occupations where they are repeatedly exposed to trauma under high levels of stress. Also at risk are people who experience trauma in childhood and people with a family history of mental illness and addictions.
Symptoms of PTSD
The ramifications of a traumatic event may be felt immediately, but PTSD is not diagnosed unless the symptoms last more than one month. Symptoms include:
Re-experiencing Symptoms
Often, people who suffer from PTSD will relive the traumatic event. This can present in different ways, including upsetting memories which can be triggered by a reminder. For instance, when a combat officer hears a car backfire and it reminds them of gunshots, or when an assault victim sees a news report and is reminded of their own experience. Once triggered, memories can cause the sufferer to react in physical and emotional ways similar to those experienced during the original event.
Avoidance and Numbing Symptoms
Individuals with PTSD may go out of their way to avoid certain triggers. They may not want to return to the site of the experience, and there might be sights, sounds or smells they will avoid. They may even stop watching TV programs that remind them of their experience.
In order to numb themselves, people with PTSD may have a hard time getting in touch with their feelings or expressing them. They may isolate themselves from others, and stop taking part in activities they once enjoyed.
Arousal Symptoms
People suffering with PTSD may feel they are in a constant state of emotional arousal. This can cause them to feel abnormally alert, resulting in difficulty sleeping, irritability and difficulty concentrating. They may feel as though they are “on guard” and searching for signs of danger at all times. This can lead to substance abuse to either heighten or dull their arousal.
Changes in Mood and Cognition
A traumatic event can result in people altering their beliefs about themselves or the world around them. People suffering from PTSD may start blaming themselves or others, and saying things such as “I should have done more” or
“People in authority can’t be trusted.” They will have a persistent low mood and decreased enjoyment of things they once enjoyed.
How can I support my loved one who suffers from PTSD?
When a family member or close friend suffers from PTSD, it can be overwhelming for family, friends and others close to the individual. It’s hard to understand the changes in behaviour, and it may feel like the individual is less affectionate or angry with you. In turn, you may be frustrated taking on more responsibilities, when the individual suffering is unable to do things they use to do. Try not to take it personally, and remember these do’s and don’ts for living with someone who suffers from PTSD:
DO
- Be patient
- Educate yourself on PTSD
- Be a good listener
- Express your commitment to your relationship
- Minimize stress at home
- Anticipate triggers and try to avoid them
- Watch for signs that your loved one is getting stressed
- Ask how you can help
- Give them space, if they need it
- Let your loved one guide you as to how they are feeling, what they can handle, and how they would like to handle their stress
- Call 911 if you feel you or your loved one is in danger of being hurt
- Make time for yourself
- Build a support system of trusted family and friends
- Set boundaries, know your limits and communicate them to your loved one, family and support team
DON’T
- Pressure your loved one to talk about their experience
- Stop your loved one from talking about their feelings or fears
- Trivialize or deny your loved one’s traumatic experience
- Tell your loved one they are weak because they aren’t coping well
- Offer advice, if you aren’t asked for it
- Take their outbursts or need to isolate personally
- Get upset with yourself if you sometimes have negative feelings towards your loved one
Men's Mental Health
Men's Mental Health
Men and women experience many of the same mental health disorders, but their willingness to talk about their challenges and feelings are very different. The perceived standards of masculinity and stigmas surrounding men seeking support for mental health disorders continue to present challenges.
In scenarios where a lack of conversation surrounding mental health related challenges exist, the absence of communication may lead to a worsening of underlying conditions and to a more acute state of the presenting disorder.
Here are some facts about Canadian men and their mental health:
- Around 10% of Canadian men experience significant mental health challenges in their life (1)
- Approximately one million Canadian men suffer from major depression each year (2)
- On average, approximately 4,000 Canadians take their own life each year, of those suicides; 75% are men (3)
- Canadian indigenous men have a suicide rate that is double that of the Canadian national average, with
- Inuit men being 11 times the national average (4)
- Gay men have a higher rate of depression, anxiety, suicidality, self-harm, and substance abuse in comparison to their heterosexual counterparts (5)
- In order of highest to lowest, Nunavut, Northwest Territories, Yukon, New Brunswick, Quebec, Saskatchewan, and Alberta have the highest suicide rates among men in Canada (6)
So why is this happening? Why are so few men seeking treatment for mental health challenges?
The current climate of men’s mental health
The current climate for men’s mental health has come to a critical point in history, where national strategies need to be made to address the increasing number of men who are experiencing mental health-related challenges.
As a society, stigmas associated with mental health are prevalent and common. Men face the added stigma that seeking help for mental health is a sign of weakness, that ‘real men’ don’t ask for help, and that talking about topics like anxiety and depression won’t help. Men often experience further bias within male counterparts with the perceived belief that mental health challenges make men a burden to others, and men should be able to control and manage their own feelings. Whatever the stigmas, we need to stop shaming men into thinking they are inadequate if they express a need to address mental health challenges or concerns. Without support and empathy, men will continue to suffer in silence and experience worsening or more acute challenges with mental health disorders.
Men aren’t unique to the stigmas associated with mental health; they may be less likely to discuss or address their concerns due to specific conditioning. As a society, we can work together to address stigmas about mental health, and encourage more people to discuss their challenges openly.
Addressing men’s mental health challenges
If we look at our individual ability to support and facilitate change, there is a lot that we can do to influence how we think about men’s mental health. Becoming an ally for those in need of, or seeking mental health support provides a safe, unbiased and supportive network for those in need.
One of the significant challenges with helping men address their mental health is encouraging and allowing them to speak openly and confidently about it. Men are typically conditioned throughout their life to not speak or act emotionally. As a supportive resource for men, it is always helpful to be aware of the signs and symptoms that a male in your life may be experiencing mental health-related concerns. Although day to day changes in behaviour are common and not cause for immediate concern, if behavioural changes continue for an extended period, typically two to four weeks it may be an indication of a mental health disorder. Here are a few visible indicators that someone may be experiencing challenges with their mental health:
- Their personality has changed from the norm, such as experiencing mood swings of experiencing mood swings, excessive anger, hostility, or violent behaviour, and having the inability to cope with minor problems and daily activities
- They are experiencing excessive anxieties or prolonged depressive states, losing interest in hobbies or social activities they were usually interested or participated in
- There has been an increased use of alcohol and/or drugs, which is beginning to affect their work and personal life
- There is a noticeable difference in their ability to think clearly and articulate their thoughts in a cohesive manner
- Their sleep and eating patterns (i.e. over or under eating) have noticeably changed, resulting in the individual seeming tired and irritable
- They may be experiencing strange or grandiose ideas, delusions, or hallucinations, which may include thinking or talking about suicide
It’s common for these indicators to be signs of physical illness as well. It’s important not to diagnosis, and seeking support from a physician, qualified medical professional, or counsellor may be a positive first step in finding help. So what can be done if you notice some of the above signs and symptoms?
How to support men’s mental health
With a greater understanding of the challenges men face when it comes to mental health, and given the various signs and symptoms that your male counterparts may exhibit, what are the actions that you and/or your organization should be doing to support men’s mental health?
- Become better informed. Understanding what men may be facing when it comes to mental health is the first step in supporting them. Reaching out to local men’s health organizations is a great way to further your learning.
- Ask what you can do. Mental health-related challenges can be difficult for anyone to talk about, so simply asking the question can be a significant step in providing the right support to this individual.
- Be there to listen. It takes a lot of courage for someone to open up about their mental health. Listening can be one of the most powerful ways to help someone, as it allows the individual to process and share their challenges.
- Don’t blame or judge. Judgement or blame can increase the challenges someone is already facing and may decrease their willingness to share or seek support. The best support you can give is being empathic and compassionate.
- Guide the person to appropriate supports. You can either direct them to their Employee and Family Assistance Program (EFAP), local support groups, a counsellor or a therapist. Although you cannot determine severity, ensuring the individual is safe and aware of options including out-patient and in-patient treatment facilities for those in need are key elements in taking the first steps towards getting help. But always ask first.
- Be optimistic and encouraging. Reassure the person that this is a medical issue and that they are not alone in what they are experiencing. Where possible, provide the time, access to treatment and support needed.
- Take care of yourself. You cannot support anyone with mental health challenges if you are emotionally drained. Protect your physical and emotional health above all.
Men aren’t unique to the stigmas associated with mental health; they may be less likely to discuss or address their concerns due to specific conditioning. As a society, we can work together to address stigmas about mental health, and encourage more people to discuss their challenges openly. The more we become comfortable talking about these challenges, the healthier our society will be. Support the men in your life by being an advocate for reducing stigmas around mental health, and being a voice for them when they need you the most.
References
- CMHA. (n.d.). Men and Mental Illness. Retrieved August 21, 2018, from https://cmha.ca/documents/men-and-mental-illness
- Sunnybrook Health Sciences Centre. (2016, December 01). We Should Be Talking About Men’s Mental Health. Retrieved August 21, 2018, from http://health.sunnybrook.ca/men/mental-health-depr…
- Health at a Glance. (2017, June 16). Retrieved August 21, 2018, from https://www.statcan.gc.ca/pub/82-624-x/2012001/art…
- Crawford, A. (n.d.). Suicide among Indigenous Peoples in Canada. Retrieved August 21, 2018, from http://www.thecanadianencyclopedia.ca/en/article/s…
- CMHA. (n.d.). Policy Papers on Equity. Retrieved August 21, 2018, from http://ontario.cmha.ca/documents/lesbian-gay-bisex…
- D. K. Macdonald (2016, September 12). Canadian Suicide Statistics 2016. Retrieved August 21, 2018, from http://dustinkmacdonald.com/canadian-suicide-stati…
Re-introducing Homewood Ravensview
Re-Introducing Homewood Ravensview

We are pleased to announce the opening of Homewood Ravensview on May 22, 2019. Ravensview will bring Western Canada its newest, private inpatient treatment facility for adults, including young adults (19+) who need immediate support for mental health and addictive behaviours (including substance use disorders and/or ‘behavioural addictions,’ like gambling addiction, gaming addiction, and sex addiction, etc.). In fact, it’s the first and only private inpatient mental health facility in Western Canada. The site on Vancouver Island, the specialized programming, and the unparalleled expertise of Ravensview’s caring staff creates an innovative therapy and healing experience for those seeking help.
Homewood Ravensview sits within the territory of the WSÁNEĆ people, atop a mountain known as ȽÁU,WELNEW or ‘place of refuge’. It’s wrapped in the beauty and serenity of the forest, with vistas that look out to the ocean. It’s a sacred place. Saanich elders tell the story of their ancestors, who sought refuge on top of the mountain, during a great flood. They tied their canoes to a tree at the mountaintop, to escape the flood. After being stranded for many days, they saw a raven that carried a twig. The people recognized this as a symbol of hope: it showed that the flood had ended. Emerging from their sanctuary, the people gave thanks to the mountain for helping them survive and providing them with a new beginning. Ravensview honours this WSÁNEĆ history, and it forms the inspiration for everything we are doing at the facility to help people in need.
With Ravensview, Homewood has taken its 135 years of clinical experience with proven therapy programs and innovative treatment practices along with therapeutically designed physical spaces and integrated structures to create a unique treatment experience. Clients in recovery live at Ravensview as part of the healing community for periods of six to eight weeks. With all of our programs, family members and significant others are included as part of the treatment process to help bridge understanding and ensure recovery supports are in place during and after a stay. We provide family education workshops as well, and communicate with the client’s family (if the client wishes) to support a complete and lasting recovery.
The treatment programs at Ravensview have been developed in a novel format. Each client is assigned into a specific group based on demographic and lifestyle factors. There are four core streams of programming within Ravensview.
- The Cornerstone Program helps adults over the age of 26 with a wide range of mental health and addiction disorders. Treatment is customized for each person’s unique needs, and the specific problems they want to address. The program is built on proven care philosophies, and evidence-based psychotherapy models, including Cognitive Behavioural Therapy (CBT) and Dialectical Behaviour Therapy (DBT). Recovery focusses on both physical and emotional health – a wholistic approach to each client.
- The Guardians Program focusses specifically on the needs of first responders, people serving in the military, and veterans of these groups. It recognizes that the experiences these individuals have had in their roles, and the exposure to traumatic situations they have often faced, creates unique challenges that require specifically designed, evidence-based treatment to facilitate the recovery process.
- The My Path Program for young adults (aged 19-26) sets a course to help each client understand how their issues are affecting their lives, how they are not alone in their experiences. The program uses evidence-based practices to help each client develop the skills and tools they need to continue to maintain psychological health, as they move through adulthood. Treatment for anxiety and mental health disorders is complemented with work that helps with issues of identity, life direction, and healthy social relationships.
- The Vanguard Program is designed for professionally-accomplished people who are facing specific challenges. Executives, professionals and entrepreneurs from both the private and public sector have many social and personal expectations and pressures that are unique and specific (including professional stress, burnout, and juggling the responsibilities of professional decision-making), which affect their ability to function over time. The program helps them address their challenges and issues that may be affecting their performance.

A day at Ravensview
At Ravensview, each client is recognized as an individual person, who has specific life goals and goals for treatment. Each client’s therapy program is customized for their specific treatment needs, with individual and group therapy sessions in the morning and afternoon. Care teams are always close at hand. Clients also participate in innovative programs including: expressive art therapy, music therapy, and horticultural therapy – which support their personal, social, emotional and physical well-being. The facilities are modern, spacious and relaxing. There are delicious meals to enjoy, and time for socializing with others, as part of the community. There are also many opportunities to explore and become immersed in the healing offered through the facility’s natural surroundings, through access to the extensive trails on Ravensview’s grounds, and the opportunity to participate in innovative recreational therapy offerings. Numerous studies have shown that the sensory experience of “taking in the forest…even a small amount time…can have an impact on our health” (Dr. Quin Li, 2018, TIME).
Why does a stay at Ravensview work so well?
Changes and recovery take dedicated time, focus and commitment. The intensive experience is a chance to step outside of the day-to-day obligations and live differently. Programs leverage proven techniques and provide clients the tools they will use throughout their recovery process. We also involve family members and significant others so they can understand how to best continue to support what’s been developed here after someone returns home.
How does someone come to Ravensview for treatment?
We are a new private treatment facility, we don’t currently have a waitlist. A doctor’s referral isn’t needed to attend a program. If you think that a stay with us could help, contact us to learn more.
