Suicide Prevention: Uncovering the Signs
Suicide Prevention: Uncovering the Signs

During these unprecedented times of COVID-19, the importance of mental health and our overall well-being has received more attention than normal. Throughout the pandemic, people have felt the overwhelming sense of loneliness, isolation and experienced multiple disruptions in their daily routine. The added economic concern, with realized job loss or threat thereof, has layered new realities and complexity to our individual and collective mental health. Although not necessarily the primary cause for one to consider ending their life, COVID-19 has become a contributing factor that influences one’s decision to consider suicide.
On average, we’re spending more than a third if not half of our waking hours at work. Colleagues often become friends rather than just colleagues and will offer you glimpses of their inner lives. Suicidal thoughts and plans are the last thing you would expect to be shared. However, what if you become aware that a colleague is contemplating suicide?
In this article, we’ll be looking at:
- What are the predisposing and contributing factors of suicide
- What are potential signs of suicidal risk in a co-worker
- How to provide support while respecting confidentiality and safety issues
- How to promote self-care and seek outside support if needed
But first, some facts…
For every death by suicide there are 20 to 25 attempts, 5 self-inflicting injury hospitalizations and 7 to 10 people deeply affected by grief.
On average, suicides claim the lives of 12 Canadians per day. In 2015, 3,269 Canadian men and 1,136 women died by suicide. (1) However, women make up to 3 to 4 times more suicide attempts than men. The actual suicide rate for women has risen by as much as 50% from 2000 to 2016 in the U.S. (2) and a similar trend has also been observed in Canada. Overall, the prevalence of suicide is growing. According to Fardous Hosseiny, the national director of research and public policy at the Canadian Mental Health Association, the percentage change over 2011 and 2015 shows an increase of 12% in males and 15% for women. The largest population of suicides in Canada are from working aged men and women between the ages of 30 to 64 with a peak occurring between 45 and 59. (3) The suicide rate among the U.S. working-age population increased by 34% between 2000 and 2016. (4)
Workplace suicides have also increased. Approximately 1,719 male and female workers ended their lives on the job in the U.S. between 2003 and 2007. (5) In 2016, the American Bureau of Labor Statistics reported a steady increase in workplace suicides from 2007 to 2013. In 2018, the Mental Health Commission of Canada published a study that found Canadian employees reported workplace stress as the primary cause of their mental-health concerns. (6) Steve Bittle, an associate criminology professor at the University of Ottawa states that between 10 and 17 per cent of annual suicides in Canada could be classified as work-related, representing a range of 400 to 800 fatalities each year. (7)
In November 2018, the CDC (Centers for Disease Control and Prevention) reported that the top 3 major occupational groups by suicide rate among males in 2015 were:
- Construction and Extraction
- Arts, Design, Entertainment, Sports and Media
- Installation, Maintenance, and Repair
For women:
- Arts, Design, Entertainment, Sports and Media
- Protective Service
- Healthcare Support
For both genders, the lowest suicide rates in 2015 were observed in education, training and library occupations.
In general, occupations with higher suicide rates involve one or many of the following factors: easy access to lethal means, exposure to chemicals, high workplace stress and risk of trauma, job insecurity, low wages, inconsistent work schedule and isolation in the workplace.
Rising workplace suicide rates shouldn’t come as a surprise in an era crippled with progressively increasing levels of pressure and stress among employees. Now the added complexity of COVID-19 has created new factors that influence the rising statistics. According to the HR Digest, the obsessive focus “on targets and deadlines, race for profits and excessive individualization as well as informal competition amongst colleagues are some of the causes of suicidal tendencies. They lead to psychological problems in the workplace which have a negative impact on the way employees work.”
When a suicide does occur, work and/or business related colleagues can be emotionally impacted with feelings ranging from anger, grief and guilt. These feelings can last far beyond the initial shock and reaction time span. Feelings and reactions may also surface within colleagues who weren’t close to the employee who took their own life. Often, death by suicide leads to rumors and speculation about why it took place. These rumours may include work-related factors and could potentially affect the morale of employees.
Predisposing and Contributing Factors
Causes for suicide are a complex cocktail of factors, including relationship breakdowns, financial difficulties, chronic physical illness, major losses, major social disruptions or a lack of social support. Some factors can be work and career related. It has been found that for every 1% increase in unemployment, there is a 0.79% increase in the suicide rate. (8) During the Great Depression, the suicide rate in America increased by 21%.
A common predisposition is an underlying mental health disorder, as 60% of completed suicides involve people dealing with a diagnosed depression. Moreover, 90% of people who take their own lives suffer from a mental health disorder. (9)
When professionals estimate the risk of suicide among employees, they will take into consideration some of the following predisposing factors:
- Access to lethal weapons
- Past suicide attempts
- Capacity to hope for positive change
- Self-help capacity, including diet, quality of sleep, medication and professional follow up
- Chronic mental health suffering and/or physical pain
- Self-control and impulsivity
- Substance usage and/or abuse
- Support network, which serves as a protective factor.
Uncovering the Signs
Depending on how close you are to a co-worker, you may or may not know of the above predisposing factors but some signs can give you hints as to the potential risk of suicidal thoughts or plans. None of these, on their own, can reveal suicidal risk, but a combination of some of the following signs can reveal a significant level of distress within your co-worker. About 75% of those who die by suicide do exhibit some suicide warning signs. 10
Work-related signs or situations to look for are isolation, performance and stress-related anxiety, conflicts with management or colleagues, job insecurity, intense expressions of job dissatisfaction, deep and long-lasting fatigue, workload issues, and presenteeism or absenteeism. It’s important to recognize that some of the previous symptoms can also be traced back to personal problems affecting the well-being and mental health of a colleague. Mental health disorders influence feelings, thoughts, behaviour and abilities. Employees dealing with a disorder may show losses in confidence, concentration and patience. It might impair their decision making, judgement and people skills. Their personality can be altered and subject to mood swings and extreme shifts in behaviours and attitudes.
More typically linked to suicide are comments on being a burden to others who they say would be better off if they weren’t there; or employees becoming suddenly very happy after a depression or despite everything crumbling down around them. More obvious warning signs require more immediate action, such as someone expressing the desire to die or to end their life and having a plan to do so. (11)
It’s estimated that up to 25% of people do not exhibit signs before ending their lives. It’s important not to blame yourself or others if a colleague completes suicide without any visual or behavioural cues. However, if you recognize any of the signs mentioned earlier, don’t hesitate to engage in a conversation with your co-worker. If you happen to be right, starting that conversation might just save your colleague’s life.
How to Provide Support
If you approach a colleague you believe might be suicidal, tell them you’ve noticed changes in their behaviour. Be respectful and share your concerns. Ask if the person is okay. It’s normal to feel uneasy and it can indeed be scary. But asking someone about suicide doesn’t put the idea in their head. Instead, according to the Ontario Suicide Prevention Network (OASP):
- It breaks isolation which can distort their fears, hopelessness and embarrassment.
- It breaks the silence and sends a powerful message that they are not alone, that you care and that it’s okay to talk about their thoughts and feelings.
- Opening up a conversation about suicide is the first step towards hope and almost always helps reduce the risk.
- It lets people the opportunity to let their fear out and to consider and talk about other options. Suicide is often less about wanting to die, and more of a feeling or belief that they have run out of options.
Be cognizant of the individual’s right to privacy and never jump to conclusions. However when you genuinely believe there is a risk of suicidal thoughts or plans:
- Don’t hesitate to ask your colleague directly if they are having difficulties. If the answer is yes, ask if they have thoughts or plans of suicide.
- If they do have thoughts or plans of suicide, first acknowledge that this is serious. Don’t act right away. Keep the person talking and keep listening. This shows empathy and understanding. It creates the necessary bond you need to build before you even mention outside help.
- Foster hope by exploring potential options for help. Seek to find supportive people like professionals or important persons in their lives that are well suited to identify better options. Remember, the suicidal person is seeking a way out of a painful situation. They are often in the dark and have lost hope, shedding light on a different road map can help them to recognize and consider other pathways.
- Check on prior attempts. You can ask you colleague if they has tried to hurt themselves in the past. If they have, the risk of suicide increases making it more urgent to get professional help.
- After your conversation, don’t let this rest upon your shoulders. You can express your concern about needing to get help in order to keep your colleague safe. Refer them to resources in your workplace (HR, EFAP), or to a mental health professional or a community resource, like a crisis centre.
The person has to be put in contact with the chosen resource as soon as possible. It is important that a person entertaining thoughts of suicide be linked to a well-trained professional that can perform a comprehensive suicide assessment and intervention within the day. (12) In the meantime, make sure your colleague is not left alone. Either stay with your colleague or ask if they have a close friend or family member that can be with them. Be sure to let your colleague know, they need to tell someone and seek help if risk of harm exists.
Remember that security issues always outweigh confidentiality considerations if a person is deemed in danger of inflicting imminent harm to themselves in a way that can threaten their life or the life of others.
Self-care
Providing support to a suicidal colleague is not easy. It can affect you emotionally, put you in a state of constant worry and make you feel responsible for one’s well-being. Crisis and suicide prevention centres most often offer support services for people who are themselves a support to a suicidal person. Your EFAP and HR resources might also offer such services. Your personal network of family and friends is also an important resource, but go to a professional support system first. It will make you better informed and should lift much of the weight of responsibility off your shoulders.
If you would like more information on suicide alert programs or training to develop skills in suicide intervention, many local and provincial suicide prevention community resources offer training and even workplace gatekeeper programs.
A positive aspect of COVID-19, one’s mental health has become more accessible. Free to all Canadians, Homewood Health is a proud partner in Wellness Together Canada. This online portal offering free resources, tools and mental health support services in both English and French. It can be accessed at wellnesstogether.ca or by phone by calling 1-866-585-0445.
No one is immune from suicidal thoughts and urges. If such thoughts should invade your mind, don’t isolate yourself, talk to someone you trust and ask for professional help. You don’t have to suffer in silence.
No one is immune from suicidal thoughts and urges. If such thoughts should invade your mind, don’t isolate yourself, talk to someone you trust and ask for professional help. You don’t have to suffer in silence.
References:
1. Statistics Canada, 2015, as reported by Global News. Source : https://globalnews.ca/news/4274136/suicide-rates-w…
2. Dr. Hedegaard, H., Suicide Rates in the United States Continue to Increase. National Center for Health Statistics (NCHS). 2018. Source: https://www.cdc.gov/nchs/products/databriefs/db309…
3. Statistics Canada, 2015. Source : http://dustinkmacdonald.com/canadian-suicide-stati…
4. Suicide Increasing Among American Workers. Centers for Disease Control and Prevention (CDCP) press release. 2018. Source: https://www.cdc.gov/media/releases/2018/p1115-Suic…
5. American Bureau of Labor Statistics (ABLS). Source : https://www.thehrdigest.com/workplace-suicides-ris…
6. Canadian employees report workplace stress as primary cause of mental health concerns. Mental Health Commission of Canada. 2018. Source: https://www.mentalhealthcommission.ca/English/news…
7. Job-related deaths in Canada dramatically under-reported, study suggests. CBC News, January 29, 2019. Source: https://www.cbc.ca/news/canada/workplace-fatalitie…
8. Stuckler,D. et al. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. The Lancet. 2009. Source: https://www.thelancet.com/journals/lancet/article/…61124-7/fulltext
9. Public Health Agency of Canada, 2016. Source: https://www.canada.ca/en/public-health/services/pu…
10. Source : http://www.suicide.org/suicide-warning-signs.html
11. American Association of Suicidology, 2017. Source: https://www.suicidology.org/resources/warning-sign…
12. LivingWorks Canada, 2007. Source : http://www.ospn.ca/index.php/suicide-prevention/su…
Moral injury in healthcare and the role of self-care
Moral Injury in Healthcare and the Role of Self-care

The traumatic legacy of the pandemic continues to impact the mental health of Canadian healthcare workers who put their lives on the line. Practicing self-care can help them heal.
July 24 is Self-Care Day, a day to recognize the importance of self-care in empowering people to look after their own health. For healthcare professionals in Canada, it’s a day to explore the ways in which self-care can play a role in helping to manage the toll that this important work can take on their mental health.
Dr. Tara Riddell is a psychiatrist for the Addiction Medicine Program and the physician wellness lead at the Homewood Health Centre, a leading inpatient treatment facility in Guelph, Ontario, that focuses on mental health, trauma, and addiction. She began exploring the relationship between mental health and self-care early in her career.
“In medical school, I started my research with the goal of reducing stigma related to mental health amongst the general population,” she explained. “But I soon recognized that this was a significant issue for myself and my healthcare colleagues, who have high rates of burnout, depression, anxiety, and suicide risk. I began to think about how I could take care of myself throughout my career journey and what other healthcare professionals may need to feel well and fulfilled in the work that we’re doing.”
Stress management for healthcare professionals has always been a challenge, but when the pandemic struck, the situation rose to crisis levels.
 Moral injury: The pandemic legacy
Moral injury: The pandemic legacy
In 2020, psychological distress in healthcare began to make headlines. As healthcare professionals all over the world risked their lives to continue delivering care under trying circumstances, their mental health suffered, and the rates of moral injury soared.
Moral injury is a type of stress caused when a situation forces a person to behave in ways that go against their moral code. Its impact on mental health is profound, and it can result in depression, anxiety, and post-traumatic stress disorder (PTSD) for healthcare professionals.
According to data collected in 2022, Canadian healthcare providers were exposed to a host of morally injurious events during the pandemic, including watching their patients die alone, witnessing patient harm, being exposed to bullying and violence, not having access to adequate resources and personal protective equipment, and coping with increased workloads and decreased staffing. In one study, a staggering 81% of Canadian healthcare workers said they were exposed to an unethical culture, 55% said they were exposed to a low psychosocial safety climate, and 50% said the quality of care was hindered.
As a result, the rates of moral injury for healthcare professionals in Canada rose dramatically. An online survey of Canadian physicians conducted in 2020 found one-third of respondents had considered leaving or previously left a position because of moral distress and another one-third met the criteria for burnout syndrome. In another survey of Canadian healthcare workers conducted in 2022, 25% had considered leaving their profession due to moral distress, 25% met the criteria for PTSD, and 60% had significant levels of depression.
A resistance to self-care
Dr. Riddell is quick to stress that solving the issue of moral injury in Canadian healthcare requires systemic change, including more resources, a bigger workforce, and improving the coordination of care. But she is also a strong proponent of practicing personal self-care as a way to manage stress and prevent burnout and moral injury.
However, healthcare professionals have a tendency to resist this approach. “Healthcare is not a culture that has been compassionate to our own vulnerability or suffering or perceived weakness, or even the disclosure at work of mental health challenges or concerns,” she said. “Sometimes it can be very challenging for health care providers to engage in self care, because we feel guilty for it, or we feel it is selfish. But in order to be at your full capacity to help others, you need to take care of your own needs first.”
From shame to acceptance
Removing the stigma around mental health is a crucial part of the process. Ironically, healthcare workers who treat their own patients with tremendous understanding often feel shame around their own mental health issues.
But extending the same sense of compassion to ourselves that we extend to our patients is the foundation for effective self care. Dr. Riddell said that when we see the difficulties or challenges we experience as part of a shared human experience, it can reduce the stigma and break down barriers.
“It allows me to have more open conversations with colleagues about something that’s weighing on me and to recognize that I’m not any ‘less-than’ as a health care provider for having some of these challenges. It helps me shed some of the shame and do a little bit of internal healing.”
Healthcare Salute, a resource for healthcare professionals who may be experiencing or at risk of moral injury, provides a helpful mental health model to help people self-assess their mental health and determine the actions they can take to improve it. The model is also intended to reduce the stigma around mental health issues by placing the full range of experiences on a continuum.
The Mental Health Continuum
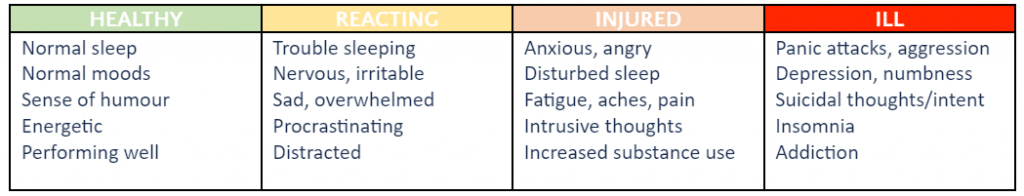
(This table is condensed and adapted from the Mental Health Continuum Model developed by Healthcare Salute. See the full continuum here.)
 Five ways to practice self-care
Five ways to practice self-care
Dr. Riddell believes that every healthcare professional can benefit from practicing self-care, no matter where they fall on the continuum of mental health.
“I often use the image of an internal tank,” she explained. “Through personal and especially professional responsibilities, our tank has lots of little drains. When our tank becomes depleted, we begin to experience greater challenges, and that’s where we may experience burnout or other mental health concerns. Self-care is a way to help refill our tank, or at the very least slow some of those drains.”
Dr. Riddell recommends these simple self-care tactics as a way for healthcare professionals to make small changes that can protect their mental health and replenish their internal tank.
Take ten. “I think everyone in healthcare has skipped a meal or a snack break or a bathroom break. Sometimes self-care means saying, ‘I may be late, but I need to take care of a basic need. If I take ten minutes to have a snack or lunch, I’m going to feel better and I’ll be able to be more present with the person I’m meeting with next.”
Try mindfulness. “In Homewood Health Centre’s Addiction Medicine Program, many of our healthcare providers incorporate mindfulness into their day. In times of heightened distress, they utilize deep breathing, attend to their own emotions, and practice ways of grounding themselves.”
Go offline. “My colleagues are increasingly finding ways to set limits on the work we do. I’m seeing staff identify when they’re going to be offline and indicate that they won’t be responding until a later date so that they have that protected time to recover.”
Reach out. “Social connection and engagement, especially with people who are also going through similar experiences, is an important way to foster self care. Social well being is one of the components of our wellness.”
Set priorities. “Increasingly, for all of us, time is a very scarce commodity. I try to think about how I’m using my time, and whether the things that are taking up my time are ultimately aligned with my core values. If they are, I’m more likely to feel a sense of enjoyment from doing it or a sense of fulfillment and meaning. And that helps me refill my tank.”
From “work warrior” to “wellness warrior”
People choose careers in healthcare because they want to nurture the health of others, but the soaring rates of moral injury for Canadian healthcare providers has shown that we’re not always as attentive to our own health. While self-care can’t mend a healthcare system in crisis, it can help those who work within it to protect their precious mental health.
“In our culture, we’ve often celebrated the work warrior, the person who is always taking on new challenges, never stops, and sacrifices their own needs,” Dr. Riddell pointed out. “Maybe we should be celebrating people who are prioritizing their wellness because they know that’s what they need and is going to be beneficial to their team and to patients.”
More self-care insights and ideas
An ongoing Canadian national study is now investigating the causes and impact of moral injury in Canadian healthcare professionals. The study involves a collaboration between Homewood Health, which has donated funds and expertise, the Homewood Research Institute, McMaster University’s Department of Health Sciences – Psychiatry and Behavioural Neurosciences, Atlas Institute for Veterans and Families, St. Joseph’s Healthcare, Western University, IDEaS, and the Public Health Agency of Canada.
As part of the project, Healthcare Salute was launched to share information, resources, and stories to help HCPs get the support they need to connect, self-assess, and practice self-care.
Trauma Informed Collaboration
Trauma Informed Collaboration

We refer to the strong emotions that can unexpectedly affect our ability to maintain our steady state as trauma. Researchers continue to learn how our bodies can hold onto the memories of these traumatic events, even those that may have occurred very early in our childhood. Unfortunately, “few people go through life without encountering some kind of trauma” through no fault of their own. (1)
However, we can change how we interact with others to be more trauma informed. When we are willing to develop an awareness that the prevalence of trauma is significant and decide to operate with that knowledge and consideration, we can find more success in our interactions and collaborations with others.
This article will explore some of the fundamentals of trauma informed collaboration as a respectful, supportive approach that helps build resilience.
What is trauma?
Many people “mistake ordinary hardship or distress for genuine trauma”, which can lead to them start using the word, trauma, as they reflect on various life incidents and memories.(2) Not every difficult situation is categorically traumatic, and not all traumatic events will be debilitating. Most of the time, we can move beyond the initial feelings that these bad experiences stir in us. When these experiences don’t easily fade into memory, they could be viewed as causing longer-term harm.
For something to be classified as traumatic in the psychological sense of the definition, the experience is:
- Out of the person’s control
- Sudden and unexpected
- Harmful or life-threatening
- Damaging to a person’s sense of safety
- Responsible for creating overwhelming vulnerability (3)
Trauma affects the body’s sympathetic nervous system by creating a state where it perceives it is constantly at risk and should be ready to respond to threats at any moment. Living with this kind of hypervigilance means that the body’s usual fight, flight and freeze responses are always activated. The stress hormones and adrenaline our bodies produce continue to circulate rather than follow the expected path of clearing out of our systems when the crisis ends so that we can return to a more relaxed state.
Researchers like Dr. Bessel van der Kolk and Dr. Gabor Maté, who have studied and helped to classify the many different types of trauma, have shown that over time, unresolved or even unconscious trauma disturbs both physical and emotional functions. These disruptions can cause everything from pain and sleeping problems, to chronic illness and severe emotional disturbances that affect someone’s sense of who they are and their relationships.
It may be helpful to realize that trauma can: (4)
- Affect as a single event or repeated occurrences of events over time
- Arise from interpersonal relationships of people who know each other
- Influence developmental stages and patterns of emotional, social, and psychological growth
- Be political in nature, threatening people’s lives, beliefs, culture, and livelihoods
What is trauma informed collaboration?
Trauma informed collaboration is an approach you can adopt as a regular part of how you interact with people daily. It means that you acknowledge and are aware of and have an appreciation that inputs – even of the most seemingly innocuous nature – can create sensory overloads in people that are traumatic responses. When someone reacts unexpectedly, it can be challenging to understand why. Sometimes it can turn a situation into one that is unintentionally counterproductive and can damage our relationships and, potentially, even future interactions. By becoming trauma informed, we can influence the outcomes of our interactions so they have the potential to be more consistent, positive, and productive for everyone.
Is this what it means when we hear something is triggering for someone?
A trigger is an association someone makes that can inadvertently kick-off “re-traumatizing interactions” that cause them to experience a “dysregulated” or intense stress response. (5) Being triggered means someone is re-experiencing trauma. It isn’t just being “uncomfortable “or sensitive or feeling that something is “rubbing you the wrong way.” (6) A person may only be aware that something will necessarily act as a trigger for them once it happens.
Being more trauma informed, that is, aware of how far-reaching trauma can be, means that we can become more attuned to signals in people’s body language that indicate someone is displaying a traumatic stress reaction.
Here’s what you might notice: (7)
- A shift in someone’s posture where they appear more nervous, uneasy, or afraid by shifting their position frequently, withdrawing or even turning their body away from an interaction.
- Trembling fingers, clenching and unclenching of fists, fidgeting, or using something physical that is nearby to create a protective barrier (such as a bag, pillow or book).
- Self-soothing gestures such as putting a hand on their head, neck, or lap.
- Rapid and quick facial expressions such as
- oraised, lowered, or furrowed eyebrows
- ofrowning or lowering of lip corners, pursed lips, or lip biting.
- Reluctance to make eye contact, looking bored, off to the side, or off in the distance.
- Crossed arms and legs, tapping and jiggling feet.
- A higher-pitched tone of voice, more rapid speech than usual, or speaking slowly and quietly or with definitive emphasis on certain words.
Why is trauma informed collaboration important?
Operating with the knowledge that most people have experienced traumatic events is a supportive approach that actively demonstrates that you are caring and compassionate about your connections and relationships with others in your own life. It also is a way to influence interactions, experiences, and environments to make them healthier at home, in the community, or at work. You might help someone who is having trouble regulating their emotions or reduce the chance that they could display challenging behaviours.
Developing your trauma informed approach takes time. As you learn, conscious practice will help you to build better relationships. More and more healthcare professionals are adopting this approach as a standard of care because they realize the benefits. You may have heard it referred to as person-centred care. (8)
How does the prevalence of trauma affect people’s experiences of seemingly ordinary events?
It may be surprising to learn how significantly trauma affects nearly everyone.
- 70% of U.S. adults have experienced some traumatic event at least once in their lives (9)
- 75% of Canadians will experience at least one traumatic event in their lifetime (10)
- 1 in 10 people in Canada have been diagnosed with PTSD (11)
Often, people display symptoms of trauma in their interactions with others. These can present as: (12)
- Physical changes
- Headaches, heart rate increase, sweating
- Exhaustion, loss of appetite, loss of libido
- More susceptible to illness
- Constipation/diarrhea
- Hypersensitivity or hyperawareness (to sounds and/or touch)
- Harmful indulgences (alcohol, drugs, food)
- Emotional changes
- Fear, depression, anxiety, panic
- Extreme mood swings, rage, anger
- Withdrawal or isolation
- Guilt, blame, shame
- Loss of interest in regular activities
- Flashbacks or nightmares (PTSD)
- All of these emotional changes could stem from a PTSD diagnosis,however, some or few people go on to develop what we consider PTSD (13)
Why is it essential to adopt a trauma informed collaborative approach?
This approach aids our ability to respond to stressful situations in healthy ways. It might help to think about it using these five words: (14)
- Realize that stress and trauma happen to all of us.
- Recognize that our reactions are attempts to feel safe again.
- Respond with understanding, compassion, and patience every time.
- Resist re-traumatizing to boost emotional safety and avoid triggering events proactively.
- Resilience helps keep the focus on people’s strengths.
By adopting principles founded in safety, empowerment, trust, transparency, collaboration, supportive help, and attentiveness to historical and cultural issues, you’ll become more confident in yourself and those you are interacting with. Think about how this approach could be beneficial for equity deserving groups, such as the LGBTQ2S+ community, and actively work to address misogyny, racism, and marginalization.
Trauma informed collaboration helps you develop healthy and appropriate boundaries. It allows you to intentionally lead from a place of empathy in all your interactions. It’s a powerful tool that can alleviate or eliminate discrimination, promote understanding, and support harmony in co-existing despite our differences.
References:
1. Psychology Today Staff (n.d.). Trauma. Psychology Today. Retrieved, May 19, 2023 from https://www.psychologytoday.com/ca/basics/trauma
2. Ibid.
3. Ibid.
4. Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
5. Dubé, Kate, LCSW. (2021 July 22) Trauma Informed Care: What is it and Why is it Important? FOOTHOLD Technology: Mental Health. Retrieved May 19, 2023 from https://footholdtechnology.com/news/trauma-informe…
6. Cuncic, Arlin. (updated 2022 March 10). What Does It Mean to Be ‘Triggered’ – Types of Triggering Events and Coping Strategies. Very Well Mind.com. Retrieved May 19, 2023 from https://www.verywellmind.com/what-does-it-mean-to-…
7. Good Therapy (updated 2019 November 1). What Is Your Client’s Body Language Telling You? ˆ Good Therapy.org. Retrieved May 19, 2023 from https://www.goodtherapy.org/for-professionals/mark…
8. Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
9. The National Council for Behavioral Health (n.d.). How to Manage Trauma. The National Council.org. Retrieved May 19, 2023 from https://www.thenationalcouncil.org/wp-content/uplo…
10.Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
11. Ibid.
12. The National Council for Behavioral Health (n.d.). How to Manage Trauma. The National Council.org. Retrieved May 19, 2023 from https://www.thenationalcouncil.org/wp-content/uplo…
13. Homewood Health eLearning program: Trauma Informed Collaboration. (n.d). Developed and delivered by Crisis Management Clinical Managers.
14. Ibid.
Celebrating Pride Means Supporting 2SLGBTQ+ Mental Health
Celebrating Pride Means Supporting 2SLGBTQ+ Mental Health

June is a time for celebrating the diversity of Canada’s 2SLGBTQ+ communities. But it’s also a time to reflect on how we can nurture and support that diversity every day of the year.
The 2SLGBTQ+ community is disproportionately affected by mental health and addiction issues, and it prevents many of its members from living their best lives and reaching their full potential. For families, friends, and caregivers alike, changing the way we think about 2SLGBTQ mental health and addiction treatment and recovery can transform the outcomes.
Progress and challenges
There is much to celebrate during this year’s Pride Month. As of 2023, Canada is home to one million individuals who identify as 2SLGBTQ+, which represents 4% of the total population aged 15 and older. Three-quarters of Canadians support same-sex marriage, and 61% say they support LGBT people being open about their sexual orientation and gender identity with everyone. Just last year, the federal government unveiled a five-year, $100 million plan to support 2SLGBTQ+ communities across the country.
Yet in some ways, 2SLGBTQ+ visibility and acceptance have never felt more fragile as there is often backlash. Between 2019 and 2021, hate crimes based on sexual orientation rose nearly 60% to reach their highest level in five years.
More than ever, we need to make an effort to understand, celebrate, and make room for queer lives and identities, and that’s especially true when it comes to supporting 2SLGBTQ+ mental health and addiction treatment.
 The cost of being queer
The cost of being queer
In a perfect world, people of all genders and sexual orientations would be given equal opportunities to thrive. But the reality is that 2SLGBTQ+ Canadians still face multiple barriers to health, wealth, and wellbeing.
Many 2SLGBTQ+ Canadians live with the trauma caused by secrecy, stigma, discrimination, and fear. In addition to being the target of hate crimes, they are also more likely to experience financial distress, homelessness, and housing insecurity than heterosexual Canadians. Canadians who are 2SLGBTQ+ also have fewer job opportunities and earn significantly less than straight, male counterparts and experience frequent microaggressions at work. A lack of access to medical care, suboptimal healthcare experiences, and poorer health outcomes also diminish quality of life for queer people.
A mental health crisis
In the face of so many challenges, it’s unsurprising that the queer community sees a higher proportion of mental health and addiction issues.
Courtney Sullivan, Addiction and Mental Health Therapist and Support Coordinator at Homewood Health Centre, which is located in Guelph, Ontario and one of the largest mental health and addiction facilities in Canada, provides both outpatient and inpatient treatment for addiction and mental health. They work with clients who identify as queer, including individuals who may be experiencing homelessness, job loss, trauma, addiction, and a range of mental health issues.
“There is a lot of stigma towards the queer community,” they explained. “A lot of people have their families disown them or kick them out or withhold family support. A lot of queer youth, in particular, end up in the shelter system, which exposes them to trauma and substance use, and their mental health can get a lot more complex.”
Research shows that 2SLGBTQIA+ Canadians are seven times more likely to abuse drugs or other substances and five times more likely to have mental health issues. Sexual-minority Canadians are also approximately 25% more likely to contemplate suicide (40% vs. 15% for the general population) or have a mood or anxiety disorder (41% vs. 16%).
Treatment challenges
Not only do 2SLGBTQ+ have a higher likelihood of developing mental health issues and addictions, but their treatment journey is complicated by systemic ignorance and discrimination in the healthcare system.
According to a 2019 survey, 59% of nonbinary people were misgendered daily and only 47% felt comfortable discussing non-binary health concerns with their primary care provider. One in three said their primary healthcare provider had no knowledge about trans/non-binary health needs, and one in four did not have access to in-person spaces specific for non-binary people.
“There’s a large amount of queer people who don’t actually disclose their queerness to their health care providers,” said Sullivan. “The medical system doesn’t have the greatest history,” they continued, pointing out that as recently as the 1970s, homosexuality was classified as a mental disorder.
“People who do disclose to their doctors are often put in a position where they have to educate them about how healthcare should be delivered, which puts a huge burden on the queer community.”
It’s even more complicated for people with an intersectional identity that combines queerness with another identity that puts them at a systemic disadvantage, such as being a person of colour or an Indigenous person.
“Recovery programs and agencies and organizations really need to show their support to the queer community and signal that they are seen, that their experiences are respected, and that the facility is open to work with you,” Sullivan said.
While Sullivan advocates for big changes in the healthcare system, including hiring for diversity and developing organization-wide policies that reflect diverse perspectives, they also believe that small things can make a big difference. As an example, they described a recent situation when they brought a suicidal trans client who didn’t feel healthy at home to the hospital. Asking for help took tremendous courage, but the client was deadnamed three times in a row during the intake process, which almost made them reject treatment. (Deadnaming occurs when someone calls a transgender or non-binary person by the name they used before they transitioned. While deadnaming may be unintentional, it can feel stressful and traumatic because it questions or invalidates a person’s gender identity.)
“The hospital is supposed to be a healthy space, and most healthcare workers are well-intentioned, but systemic homophobia and racism can come out through the policies and the way things work,” they said. “Something as simple as restructuring medical charts so that gender information and preferred pronouns are easily available at a glance can change the experience. Or have care providers identify their pronouns, which is kind of like offering an invitation for that person to give you theirs too.”
S upporting 2SLGBTQ+ mental health
upporting 2SLGBTQ+ mental health
If you are a friend, partner, or family member of a 2SLGBTQ+ person exploring treatment options or actively in treatment or recovery, you can play an integral role in supporting their mental health and resilience.
For Sullivan, these communication tips can help to ensure they feel heard, seen, and supported throughout the journey.
Let them lead. “Your loved one might have a substance use issue, but if they’re not ready to hear it, don’t force it on them,” said Sullivan. “When people get scared, they make threats, like, ‘You need to get sober or else!’ But that ruins the opportunity and the trust.” Instead, let that person decide what they need and set the pace for treatment and recovery.
Keep an open mind. “Come at things with empathy and compassion. Listen to that person. Try to understand why they’re making the choices that they do.” Sullivan pointed out that for some members of the 2SLGBTQ+ community, the use of stimulants is an important part of their lifestyle and sexuality. “It all comes back down to the impact that the person’s substance use has on their life, and what that person identifies as being problematic.”
Respect their experience. “The trauma and the experiences that queer people have are different,” Sullivan explained. “Even if you’re cisgender and you get kicked out of your home, it’s still a different experience than someone being kicked out of their house because of who they are.” Respecting those differences can go a long way toward creating a space for authenticity and healing.
 Pride in mental health
Pride in mental health
Pride Month is a time to celebrate the queer community and bring attention to the challenges it continues to face. The elevated risk of mental health and addiction issues is an important part of the story, and one that Homewood Health Centre and other mental health and addiction facilities in Canada are highlighting this year. We all have a role to play in supporting and protecting the mental health of 2SLGBTQ+ individuals, and that role goes beyond raising the rainbow flag.
“We’re having a flag-raising ceremony in honour of Pride here at Homewood, but that’s just the first step,” said Sullivan. “It’s about creating intersectional representation. You want people of colour working in your organization, you want Indigenous perspectives, you want queer perspectives. Be willing to hear the experiences of the people you employ and the people you support. Find out what it is that they’re looking for.”
Learn more about LGBTQ+ mental health.
Learn how to support children who identify as LGBTQ2+.
How to be an Ally
How to be an Ally

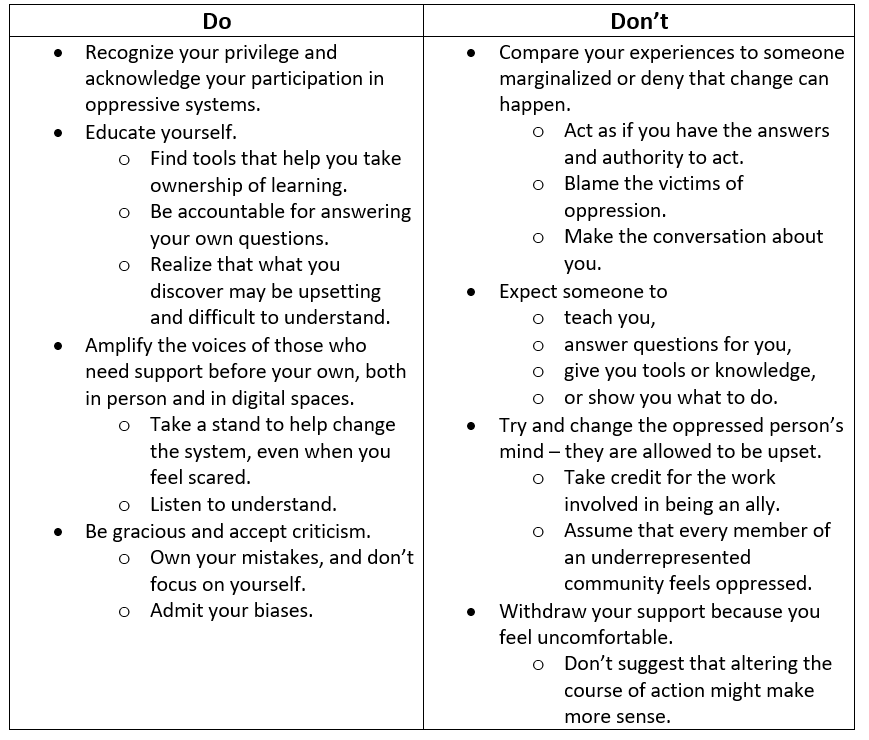
Being an ally is about far more than making a declaration. It’s a conscious, educated decision that leads someone to develop sincerity, focus on introspection, and learn about consistency.
True allies show solidarity for people whose circumstances are different and challenging. There should never be any expectation of recognition or gratitude. An ally must understand this and embrace it. Embracing allyship helps you realize how you live your life and can support earnest changes in behaviours in yourself and society that can contribute to shifts that chip away at injustices and inequities.
In this article, we will explore some of the fundamentals, clarifying what it means to make the personal decision to be an ally and why allies are necessary. We’ll also look at the actions allies can take to strengthen our workplaces and communities.
What is an ally?
An ally is someone who wants to partner with marginalized people in our society to help overturn oppression and inequities that center around topics such as race, cultural identity, gender, religion, sexual orientation, ability, and body type/appearance. Allies focus on standing up “for equal and fair treatment of people different from them” whose voices are underrepresented.[1]
Allies recognize that introducing consistency in their lives can result in solidarity with others because they approach things earnestly, knowing that the right kind of support can change behaviours and ideas. Allyship is most effective when it happens in the context of genuine relationships and everyday interactions.
A large component of being a successful ally is practicing self-awareness and self-accountability.
- An ally must acknowledge how their privilege has benefited them.
- They must be open to listening to understand and learn about the kinds of meaningful actions they can offer as a show of support for people lacking privileged advantages.
Another way to look at it is that an ally cares enough to make a conscious decision to support someone who is a member of a group that the ally is not a part of and who is having a negative experience in their life. They also recognize that allyship is not pity. When enough people decide to be allies, that’s the point where social and societal change begins to happen.
Allyship is only valuable if it’s consistent. It can also be contradictory if the ally enters a situation from a solutions-oriented perspective because they believe they know exactly how to fix a problem. The responsibility for learning about the challenges marginalized groups experience is not something for an ally to expect their marginalized contacts to offer. It’s up to the ally to seek accurate knowledge responsibly. An ally must self-educate consistently and without expecting recognition for their involvement.
Why are allies necessary?
We often adapt what we think, say, and do to blend in with the crowd. It can help us feel accepted, safe, and that we belong, leading us to behave in specific ways, like others in the group, so that we aren’t asked to leave it. Psychologist Robert Cialdini observed that “people copy the actions of others to know how to act in a certain situation. This idea stems from the assumption that if other people are doing something, it must be the correct thing to do.”[2] What’s interesting is that we tend to conform even when we observe or experience something that we know is wrong. The people around us subtly influence us: social actions and opinions are contagious, both good and bad.
Allies dare to reflect and recognize their privilege and use it to “influence inclusion and call out or challenge behaviour [that perpetuates] bias and systematic oppression based on race, gender, sexual orientation and ability.”[3]
What actions can you take to become an ally?
Being an ally comes with great responsibility. Here are some considerations:
How can you be a better ally in the community?
Being present as an ally is about consistency. Show up for all people and groups, observing that each may take a unique approach. An example of a simple action you can take is to acknowledge important holidays and milestones.
Recognize that you might be the one who needs to change or stand up for change to correct a misperception. Pay close attention to language and ideas to reflect that in conversations to show you care. Stand up to discrimination when you see it by modelling active listening. For example, take time to learn the correct pronunciation of people’s names. You could also support someone’s expertise and skills and invite them to share their knowledge within the community.
You also need to respect boundaries. Some people may adapt their behaviours for safety reasons. Don’t chastise them for doing that. Follow their lead and try to understand why they are making that choice. Think about what a shift in behaviour in the future could do that might result in a safer experience for them.
How can you be a better ally at work?
You can start by recognizing that there are inequities in the workplace that affect people’s physical and mental health significantly. These might be centred around income and lifestyle or other factors that affect the identity they portray at work and their ability to be their authentic self.
Known issues include:
- Unequal pay
- Lack of diversity
- Underrepresentation of people in marginalized groups in management/leadership positions
Remote work adds another complication. It’s easy for people to make assumptions about one another when their interactions are virtual. The lack of physical presence can introduce microaggressions that often have remote workers feeling excluded and undervalued.
Allies can help push for changes by actively advocating and participating in these approaches to ensure that concerns are discussed and not diminished.
Create space for productive discussions
Be willing to have and support uncomfortable talks, even if the topics are controversial. It holds the organization accountable for addressing Diversity Equity and Inclusion (DEI) issues, especially if HR policies are already in place.
Develop mentorship opportunities
Supporting allyship can be strategic, allowing people to become “collaborators, accomplices, and co-conspirators who fight injustice and promote equity” through the relationships that develop and actions taken during mentoring.[4] It can be the catalyst to drive change.[5]
Use a strategic and measurement-based approach
Engage in ongoing measurement to evaluate if your DEI policies are effective. This includes creating annual or quarterly plans that outline DEI initiatives that drive or align with the organization’s strategic plans; defining who is accountable for the initiatives, establishing and analyzing key performance metrics to assess the impact of initiatives and programs and incorporating on-going feedback from leaders and employees.
Change the usual ways feedback about DEI issues is collected
Allies can encourage people to share what the organization should start doing, stop doing, and stay doing. Keeping things simple can help everyone feel safe sharing their realities and bringing transparency to what is happening at work. People never want to feel like they are the only ones sharing their situations. There should be zero tolerance for inequity and discrimination.
References:
[1] Wells A. & White B. (2021 February 4) Why is Allyship Important? National Institutes of Health (NIH). Retrieved April 27, 2023 from https://www.edi.nih.gov/blog/communities/why-allyship-important
[2] Cherry, K. (2022 January 20, Updated 2023 March 5). Confirmity: Why Do People Confirm? Explore Psychology. Retrieved April 27, 2023 from https://www.explorepsychology.com/conformity/
[3] Rice, D. (2021 August 18). The Keys to Allyship: Understanding What an Ally Is and the Role They Play in an Inclusive Workplace. Diverity Inc. Powered by FAIR360. Retrieves April 27, 2023 from https://www.fair360.com/the-keys-to-allyship-understanding-what-an-ally-is-and-the-role-they-play-in-an-inclusive-workplace/#:~:text=In%20majority%2Dwhite%20societies%2C%20effective,privilege%20to%20drive%20tangible%20change.
[4] Ibid.
[5] Ibid.